Crossing finish line likely not part of learning to live with COVID
Read this article for free:
or
Already have an account? Log in here »
To continue reading, please subscribe:
Monthly Digital Subscription
$0 for the first 4 weeks*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*No charge for 4 weeks then price increases to the regular rate of $19.00 plus GST every four weeks. Offer available to new and qualified returning subscribers only. Cancel any time.
Monthly Digital Subscription
$4.75/week*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*Billed as $19 plus GST every four weeks. Cancel any time.
To continue reading, please subscribe:
Add Free Press access to your Brandon Sun subscription for only an additional
$1 for the first 4 weeks*
*Your next subscription payment will increase by $1.00 and you will be charged $16.99 plus GST for four weeks. After four weeks, your payment will increase to $23.99 plus GST every four weeks.
Read unlimited articles for free today:
or
Already have an account? Log in here »
Hey there, time traveller!
This article was published 01/02/2022 (1407 days ago), so information in it may no longer be current.
We have to learn to live with COVID-19.
It’s not a new motto — we’ve heard it from politicians and public-health officials throughout the pandemic. No one knows exactly what it means, including those who use it. What it may have meant at the beginning of the pandemic is probably different than what it means now. Either way, it is something we have to better understand.
“We have to learn to live with this virus because this virus isn’t going away,” Dr. Brent Roussin, the chief provincial public health officer, said on June 15, 2020, during one of his early-pandemic briefings.

He was right, the virus is here to stay. The question now is: how do we manage it?
We may not know precisely what “learning to live with COVID-19” means. However, we know what it isn’t. It isn’t a rallying cry to throw our hands in the air, doff our masks and drop public-health restrictions overnight. Learning to live with the virus isn’t (or shouldn’t be) a declaration that, “I’m done with COVID, damn the consequences.” That would require us to become more tolerant of death, misery and the further erosion of hospital care, which most of us are probably not willing to do.
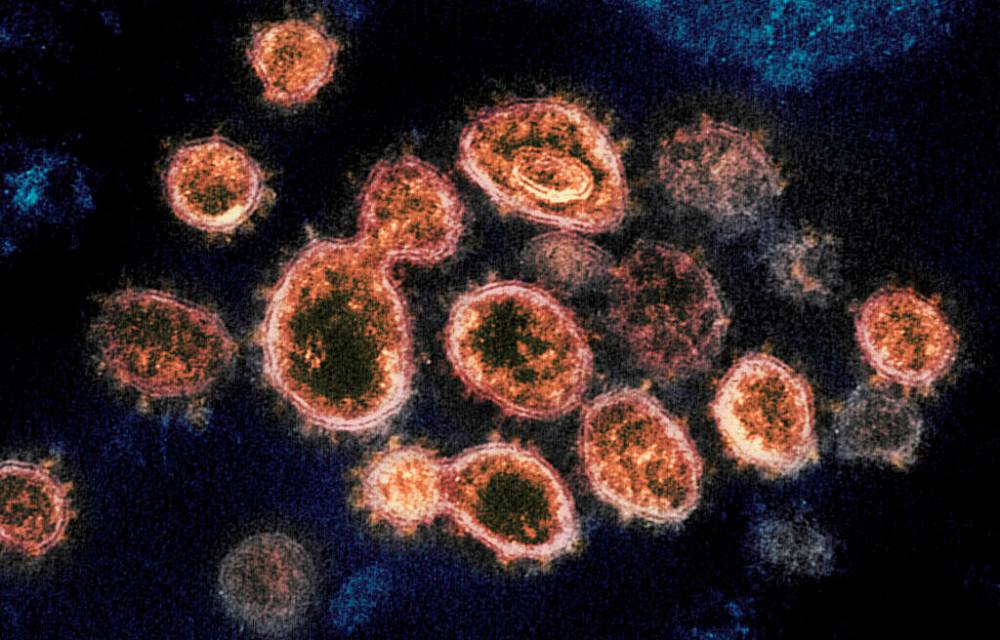
To some degree, we have already learned to live with COVID-19, mostly because we know a lot more about it than we did at the beginning of the pandemic. We’ve learned how the virus spreads (it’s airborne), that masks are an effective tool to mitigate transmission and that proper ventilation indoors can significantly reduce the spread of the virus.
We’ve learned how the virus spreads (it’s airborne), that masks are an effective tool to mitigate transmission and that proper ventilation indoors can significantly reduce the spread of the virus.
We’ve learned through clinical trials and mountains of real-world data that vaccines lower the risk of infection (even with the Omicron variant, according to a wide-ranging U.S. study released last week by the Centers for Disease Control and Prevention), and significantly reduce severe outcomes, including hospitalizations and death. We also learned that unless we distribute vaccines equitably throughout the world, the virus will continue to mutate and prolong the pandemic.
After four waves of the pandemic (possibly five, depending on how you count), we know that public-health measures that reduce physical contact between people — such as capacity limits in public places or outright closure, in extreme cases — are sometimes needed to prevent hospitals from becoming so overwhelmed they can no longer treat patients in a timely manner (as is the case now).
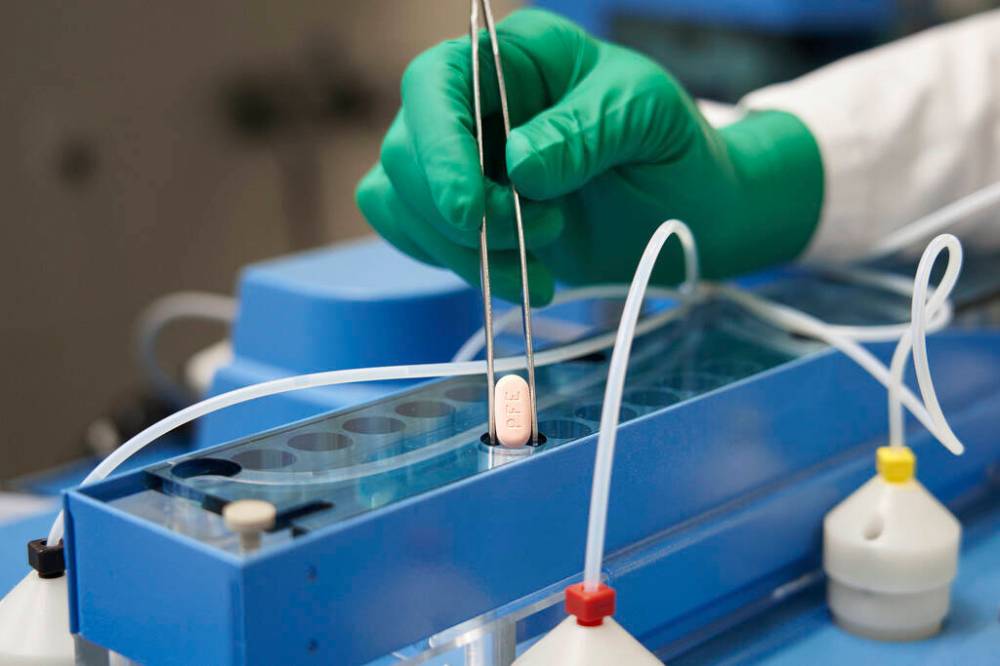
We have learned that COVID-19 can be treated with effective anti-viral drugs, such as Pfizer’s Paxlovid, which was approved by Health Canada last month.
We’ve learned a lot.
Most of what we know comes from the work of scientists, who not only brought us safe, effective vaccines and treatment options, but who continue to analyze, examine, test and re-evaluate (a.k.a. — doing science) how the virus spreads, mutates and affects our immune systems.
Sadly, we also learned how fear, misinformation and indoctrination can conspire to convince some to reject that science and impede efforts to manage the virus. It’s been one of the most frustrating and difficult aspects of learning to live with COVID-19.
While the concept of learning to live with the virus is still a bit murky (including what public-health measures will be required, both short-term and long), we have a better understanding of it now than when Roussin first uttered those words.
Learning to live with the virus means taking whatever steps are needed to protect those who can’t protect themselves and finding ways to return to normal life safely and incrementally without causing more harm than good. Those are vague terms, but with the support and ingenuity of science, they are achievable goals.
Learning to live with the virus means taking whatever steps are needed to protect those who can’t protect themselves and finding ways to return to normal life safely and incrementally without causing more harm than good.
There is no clarity beyond that. That’s life. It’s the reality of pandemics. Those who insist on a more immediate and certain path will only find themselves consumed with anger and frustration (or, in the the case of the “freedom convoy” protesters in Ottawa, rage). They will be no further ahead.
Through vaccination, natural immunity, improved treatment and non-pharmaceutical interventions, we will continue to learn to live with COVID-19 and inch our way back to normal life. Once we do, we can look back at everything we learned and take some comfort in knowing we will be better prepared for the next pandemic.
tom.brodbeck@freepress.mb.ca

Tom has been covering Manitoba politics since the early 1990s and joined the Winnipeg Free Press news team in 2019.
Our newsroom depends on a growing audience of readers to power our journalism. If you are not a paid reader, please consider becoming a subscriber.
Our newsroom depends on its audience of readers to power our journalism. Thank you for your support.