COVID-19 surge forces transfer of Manitoba patients to Ontario Thunder Bay hospital sets aside 20 beds for Manitobans
Read this article for free:
or
Already have an account? Log in here »
To continue reading, please subscribe:
Monthly Digital Subscription
$0 for the first 4 weeks*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*No charge for 4 weeks then price increases to the regular rate of $19.00 plus GST every four weeks. Offer available to new and qualified returning subscribers only. Cancel any time.
Monthly Digital Subscription
$4.75/week*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*Billed as $19 plus GST every four weeks. Cancel any time.
To continue reading, please subscribe:
Add Free Press access to your Brandon Sun subscription for only an additional
$1 for the first 4 weeks*
*Your next subscription payment will increase by $1.00 and you will be charged $16.99 plus GST for four weeks. After four weeks, your payment will increase to $23.99 plus GST every four weeks.
Read unlimited articles for free today:
or
Already have an account? Log in here »
Hey there, time traveller!
This article was published 19/05/2021 (1666 days ago), so information in it may no longer be current.
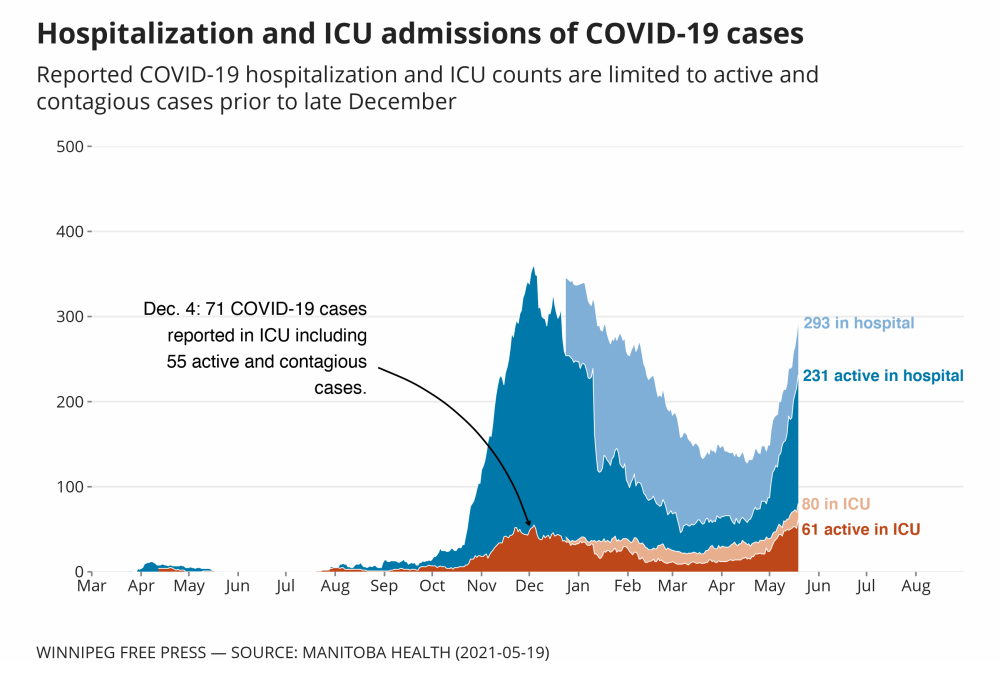
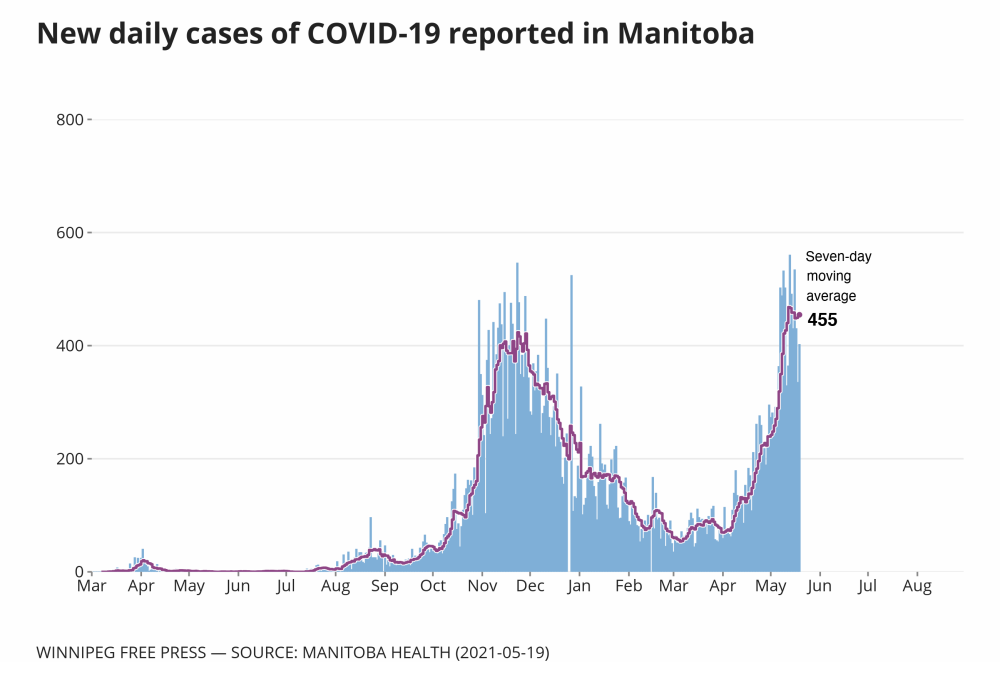
One day after the health minister suggested Manitoba’s ICU capacity could handle a surge of COVID-19 patients, the government revealed three critically ill people had been transferred to a hospital in Thunder Bay, Ont.
Manitoba ICU capacity can expand to 170 beds: health minister
Posted:
Health Minister Heather Stefanson says the province can expand to 170 ICU beds and shouldn't need a triage protocol to decide who gets a bed and who doesn't.
Shared Health announced Wednesday that multiple days of hospital admissions “far beyond” the numbers experienced during the second wave of the pandemic last fall had placed “extreme strain” on health-care staff.
During a four-day period ending Monday, Manitoba intensive care units admitted 34 patients with COVID-19 – nearly half of pre-COVID hospital critical care capacity (72).
With no let-up in the number of new critically ill patients entering hospitals, and no ability to shift sufficient numbers of ICU patients out of critical care, officials took the unusual step of transferring two stable COVID-positive patients to the Ontario city for ongoing care Tuesday, and a third was being transported Wednesday afternoon.
“These are not easy situations. These are not easy decisions that are being made. This is not an ideal situation, no question,” Health Minister Heather Stefanson told reporters.
Asked if more critically ill patients may be transferred out of province in the coming days, Stefanson said that would depend on whether the explosion in hospital admissions continues.
“This has been kind of an extraordinary surge in the last few days alone…,” she said. “Those decisions will be made on the basis of the… safety and health of those patients.”
After Stefanson spoke to reporters, Shared Health confirmed a third patient was being transferred, and a spokesperson issued a statement to say more patient transfers are being considered as “an interim measure while we work to increase staffing and build critical care capacity.”
A source told the Free Press Wednesday evening there may be as many as 20 beds available for Manitobans in Thunder Bay because more patients are expected to be transferred there.
Premier Brian Pallister was absent from the legislature on Wednesday. A spokeswoman said he and Infrastructure Minister Ron Schuler were “getting an on-site update on the wildfire situation near Carberry.”
On Tuesday, Stefanson said the province could expand to 170 ICU beds, depending on staffing, and shouldn’t need a triage protocol to decide who gets a bed and who doesn’t.
But ICU doctors are questioning whether the province has a clinical care model and enough staff to safely care for 170 ICU patients — the transfers to Thunder Bay indicate otherwise. Space, they say, is not a problem. But the number of patients can’t expand unless more nurses are brought in. Otherwise, patient care suffers.
Total ICU admissions have quickly approached the second-wave peak of 129 patients, and the number of COVID patients in the ICU has surpassed the second-wave peak of 71. There were about 80 COVID patients in the ICU Wednesday morning and nearly 300 COVID patients hospitalized in total. There are more than 120 patients in ICUs, including COVID and non-COVID patients.
“I don’t think any front-line physicians would, at this stage, tell you that there’s an ability to care safely for 170 patients in Winnipeg,” said Dr. Eric Jacobsohn, an ICU physician and cardiac anesthesiologist at Health Sciences Centre and St. Boniface Hospital.
Dr. Anand Kumar, another attending ICU physician in Winnipeg, said that level of ICU capacity expansion is purely theoretical. ICU nurses normally work one-on-one with critically ill patients because they need intensive treatment. In the second wave, nurses carried double or triple their usual patient loads and in this third wave, they’ve been doubled up for several weeks already. Realistically, they are already over-capacity, he said.
“I don’t think any front-line physicians would, at this stage, tell you that there’s an ability to care safely for 170 patients in Winnipeg.” – Dr. Eric Jacobsohn, an ICU physician and cardiac anesthesiologist at Health Sciences Centre and St. Boniface Hospital
“I don’t know what their plan is. Based on the manpower that’s currently present, we don’t have capacity. We’re in a dire situation, and in my opinion, and in the opinion of several colleagues who’ve spoken to me, they’re already seeing degradations in the quality of care and standards of care,” Kumar said.
Stefanson disagreed with a suggestion that the 170-bed figure she gave on Tuesday was a phantom number.
“When you have a surge as large as it’s been in the last few days, there’s obviously challenges, (including) moving staff around in a very short period of time,” she said.
“We are dealing with the unions and so on of those employees. Sometimes, it takes a period of time to make those transitions happen.”

Because of the overload, operating rooms and some emergency rooms have closed and staff have been redeployed to ICUs. On Monday, chief nursing officer Lanette Siragusa said 82 nurses had been redeployed to ICUs. On Wednesday, a Shared Health spokesperson said 51 nurses — who normally work at Concordia Hospital, Misericordia Health Centre, the Pan Am Clinic, Seven Oaks Hospital and Victoria General Hospital — had been sent to ICUs in Winnipeg.
There are 619 full-time nursing positions and 171 full-time support-staff positions in Manitoba ICUs, a Shared Health spokesperson said Wednesday, but it wasn’t clear how many of those jobs are currently filled. The province is in the recruitment stage to fill 60 additional ICU nursing positions.
Kumar said critically ill patients from Thunder Bay are routinely transferred to Winnipeg because it’s faster than sending them to a larger hospital in southern Ontario, but until now, Manitoba hadn’t needed to send any patients there. He said he was aware it was contemplated during the H1N1 crisis.
Asked on Monday whether transferring patients to Thunder Bay was an option, Siragusa said it hadn’t happened but wasn’t off the table.
“People have been telling us, develop ICU capacity. This government made a political decision not to invest in ICUs.” – NDP Leader Wab Kinew
“There’s all sorts of options that we need to look at if we exceed our capacity in Manitoba,” Siragusa said Monday.
NDP Leader Wab Kinew called the patient transfers “disturbing news.”
He said they are the result of the Pallister government’s failure to plan and invest adequately in health care.
“People have been telling us, develop ICU capacity,” Kinew said. “This government made a political decision not to invest in ICUs. This government made a political decision not to get ahead of the problem by doing that upstream work of training the necessary staff, allocating the necessary staff resources. And now today, we see the result.”
“It means that we are in an incredibly dangerous place.” – Liberal Leader Dougald Lamont said about the transfers
Liberal Leader Dougald Lamont said it is “unprecedented” for Manitoba to transfer such critically ill people out of province to Thunder Bay.
He noted that Winnipeg serves as a critical-care hub for a large region that includes Manitoba, Nunavut and parts of Saskatchewan and northwestern Ontario.
“It means that we are in an incredibly dangerous place,” he said about the transfers.
larry.kusch@freepress.mb.ca
katie.may@freepress.mb.ca


Katie May is a general-assignment reporter for the Free Press.
Our newsroom depends on a growing audience of readers to power our journalism. If you are not a paid reader, please consider becoming a subscriber.
Our newsroom depends on its audience of readers to power our journalism. Thank you for your support.
History
Updated on Wednesday, May 19, 2021 3:59 PM CDT: Adds four additional deaths.
Updated on Wednesday, May 19, 2021 6:57 PM CDT: Graphics and quotes added.