Deadly lessons ignored Manitoba officials, care-home operators watched Ontario, Quebec spring nightmares unfold but failed to prepare for devastation here, critics charge as virus invades facilities
Read this article for free:
or
Already have an account? Log in here »
To continue reading, please subscribe:
Monthly Digital Subscription
$0 for the first 4 weeks*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*No charge for 4 weeks then price increases to the regular rate of $19.00 plus GST every four weeks. Offer available to new and qualified returning subscribers only. Cancel any time.
Monthly Digital Subscription
$4.75/week*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*Billed as $19 plus GST every four weeks. Cancel any time.
To continue reading, please subscribe:
Add Free Press access to your Brandon Sun subscription for only an additional
$1 for the first 4 weeks*
*Your next subscription payment will increase by $1.00 and you will be charged $16.99 plus GST for four weeks. After four weeks, your payment will increase to $23.99 plus GST every four weeks.
Read unlimited articles for free today:
or
Already have an account? Log in here »
Hey there, time traveller!
This article was published 23/10/2020 (1872 days ago), so information in it may no longer be current.
Personal-care home residents tell reporters they’re scared and missing meals and baths. COVID-19 deaths hit double digits in a facility while desperate families try to find out whether their relatives are infected. Provincial officials and a private company volley questions to each other.
What played out at care homes in other provinces in the spring is repeating six months later in Winnipeg, raising questions about whether Manitoba learned anything from first-wave outbreaks in Quebec, Ontario and British Columbia.
To date, there have been 25 deaths in Manitoba care homes and more than 120 cases involving residents. Fifteen of those deaths involved residents from the Revera-owned downtown Parkview Place Long Term Care Home, continuing a trend across the country of deadlier outbreaks at privately owned facilities.
“What’s happening in the Parkview home should be a real warning to Manitoba about some of the structural factors that contribute to how large outbreaks get and how deadly they get,” said Dr. Nathan Stall, one of Canada’s leading gerontologists.
Premier Brian Pallister’s government intervened early to prevent care workers from circulating between jobs at multiple personal care homes and took steps to recruit retired nurses to deal with anticipated burnout.
But Manitoba’s staffing efforts were stepped up only this week — an inexcusable delay in time, unions charge — to reinforce depleted ranks of sick and exhausted workers. There are, currently, 14 care homes in Winnipeg dealing with outbreaks and all care homes in the area are now categorized at the code red — critical — level in the province’s pandemic response system.
Meanwhile, nurses say they still can’t get protective masks, while the health minister last week referred to deaths among long-term care residents as “unavoidable.”
A lack of transparency makes it impossible to tell whether care homes have enough staff, and how many residents are getting tested.
“In Manitoba, this catastrophic outbreak is a real warning sign of what can happen,” said Stall, who works at Toronto’s Mount Sinai Hospital . “Addressing many of those issues, expediently, is really a necessity.”
A system under strain
Canada’s first COVID-19 death occurred at a B.C. care home in early March. Since then, four-fifths of fatalities nationwide have occurred in personal-care homes. But B.C. got the situation under control much faster than was the case in Ontario and Quebec.
Care homes are particularly vulnerable to the novel coronavirus because roughly 70 per cent of residents across Canada live with dementia, making it hard to enforce physical hygiene, hand-washing and mask-wearing. Older people face more severe outcomes from COVID-19, which wreaks havoc on compromised immune systems.
Provinces regulate care homes, with widely varying standards and transparency. But across Canada, personal-care assistants are generally paid only slightly above minimum wage, often with part-time contracts that force many to work in multiple workplaces to earn a living.
“It’s back-breaking work, poorly recognized, poorly paid, undervalued,” Stall said.
“Unfortunately, like everything in COVID-19, it’s preying on the most vulnerable and neglected sectors of our society, and it’s hard to fix all these issues overnight.”
“It’s back-breaking work, poorly recognized, poorly paid, undervalued.” – Gerontologist Dr. Nathan Stall said of personal-care assistants
B.C. officials noted underpaid staff were often working in multiple facilities, likely spreading the virus before they had symptoms. In short order, restrictions were put in place prohibiting staff movement between facilities.
And that province started off in a better shape than most, with a seniors advocate flagging issues before they festered, better integration with hospital specialists and a funding structure that has homes regularly renovated. That meant a seamless response in which hospital staff trained employees — in care-homes with space to isolate patients — in infection-control protocols.
Just 25 per cent of care-home beds in B.C. are in shared rooms of two or more people, compared with 60 per cent in Manitoba, which happens to be the national average.
Meanwhile, Ontario and Quebec scrambled to draw up new connections between hospitals and care homes, many of which are substantially older and more crowded than in B.C. Before long, the Canadian Forces were called in to assist in both provinces as the numbers of deaths spiked and the situation inside facilities became untenable.
‘A domino effect’
At the beginning of the pandemic, Manitoba’s long-term care system was in a better state than those in Ontario and Quebec.
Like B.C., regional health authorities share supports such as infection-control experts who normally work in hospitals. Those authorities help analyze staffing levels and inspect care homes at least every two years.
But unlike B.C., Manitoba’s system has been repeatedly subjected to cuts in an effort to get expenditures under control. And there is a backlog of renovation plans to update outdated rooms that house multiple people amid an increase in the number of residents living with dementia and other complex health needs.
“In Manitoba we’re working with 15 years of funding shortfalls and with infrastructure needs that were basically ignored,” said Jan Legeros, head of the Long Term and Continuing Care Association of Manitoba.
“If we had begun this pandemic from a place of strength, instead of a place where we have no reserves, it would have been easier to manage.”
Manitoba care homes acted to prevent staff from working in more than one facility before the province implemented a blanket ban in April, Legeros said.
“We didn’t have the same challenge that Ontario and Quebec faced, fortunately for us,” said Legeros.
To cope with that limitation, Shared Health and regional authorities looked for surge capacity, by determining whether each facility had sufficient numbers of people who had committed to working there exclusively.
Unions support restricting employees to one site, but they argue the practice has strained a system already-stretched thin by inadequate staffing. And if that wasn’t enough, some care homes were dealing with additional shortages because staff had fallen ill or were isolating after exposure to the virus.
“We’ve got three levels of a staffing shortage going on,” said Shannon McAteer, health-care co-ordinator for CUPE, which represents care workers.
“There’s absolutely a domino effect that’s happened in all this.”
Restricting staff to one home has put some in a precarious state. Some held combined hours equivalent to 1.8 full-time jobs, to counter low wages. The province has capped compensation to just 1.3 jobs per person, effectively limiting overtime.
“In Manitoba we’re working with 15 years of funding shortfalls and with infrastructure needs that were basically ignored.” – Jan Legeros, head of the Long Term and Continuing Care Association of Manitoba
Manitoba officials established a Provincial Recruitment and Redeployment Team in the spring to identify nurses and care workers who had recently left the industry, as well as facilities that potentially could spare personnel.
The team also diverted medical staff idled by cancelled surgeries and other procedures to work on pandemic-related tasks.
The idea was to have surge capacity when care homes experienced staff shortages from booking off sick or burnout, Legeros said. Available workers were asked to look at online postings to fill spots.
The province said 320 people were recruited in numerous areas, including contact tracing, but did not provide a precise number for care homes.
The president of the Manitoba Nurses Union said 64 nurses came out of retirement.
“It’s a drop in the bucket for the shortage we’re seeing,” Darlene Jackson said.
“Knowing what we knew, seeing what had happened in Quebec and Ontario in those long-term care facilities, I feel like we should have been much, much more prepared.”
Unprotected
Manitoba’s first care-home case appeared April 3 at Winnipeg’s Poseidon Care Centre, also owned by Revera. By that point, both CUPE and the MNU had complained to the province about inadequate personal protective equipment, particularly N-95 masks.
When a Manitoba care home has COVID-19 cases, staff attempt to section off areas for those presumed positive.
In areas where the coronavirus isn’t suspected, care-workers don light-blue surgical masks, which prevent them from unknowingly infecting a resident. A gown, gloves and face shield are also used as precautions.
In a COVID-19 positive ward, care workers argue they’re entitled to an N-95 mask, which prevents the wearer from getting infected. But they often can’t get one, leading to a formal grievance this week involving 55 Manitoba health facilities.
Nurses face the same problem, and the MNU established a joint committee with employers in July to deal with PPE issues. So far this fall, It has heard every other day from a nurse whose manager has denied them an N-95 mask.
This week, Manitoba’s chief public health officer Dr. Brent Roussin cited PPE as a key factor in the province’s care-home outbreaks. Pallister has pointed to federal delays and meddling in provincial equipment purchases.
‘All hands on deck’
Manitoba is now launching a public campaign to get more workers for care-home jobs.
The move comes after the WRHA had to deploy people in roles from housekeepers to staff trainers this week to Parkview, where 26 staff and 82 residents have tested positive for the virus thus far.
In an interview, Health Minister Cameron Friesen said that’s part of Manitoba’s flexibility in reaching across its health sector to recruit people as needed.
“It’s all hands on deck, and that is why we’re saying whatever resources we can muster to assist in exceptional circumstances, we want to welcome those resources in,” he said.
While the province had encouraged retired nurses to look at online postings, Legeros said the new effort targets people with various skills.
“They’ve even established a pool, so that they will interview and hire and partner with the Alzheimer’s society and their own infection-control people, to give these staff the training they need to go into (long-term care) and other health-care facilities,” Legeros said.
The effort launched Monday, and the province said it has already hired 15 people and there are as many as 50 who’ve expressed interest each day.
Unions say they’re shocked that it has taken the province this long to act.
“We got through Wave 1, we had the whole summer to get out there and start recruiting and get people into the system,” Jackson said. “Now we’re in Wave 2, we’re seeing the numbers increase — and suddenly the government is out there recruiting.”
She noted that Ontario’s Progressive Conservative government put up $50 million to step up recruitment efforts in the spring.
Quebec hired 10,000 workers over the summer, paying them $21 per training hour and $26 for working hours, rates previously unseen across Canada — though no other province experienced as many residents’ deaths and staff losses.
Manitoba NDP health critic Uzoma Asagwara contends that the Pallister government spent too much energy on making sure the province was the first to repeal restrictions.
“As the economy was encouraged to thrive, that wasn’t matched with the resources and investments needed to ensure that folks had what they need to mitigate the spread of COVID-19,” Asagwara said.
“It’s pretty obvious now that enough wasn’t done.”
The NDP critic said the province needs to ramp up hiring and get PPE to care homes. The province still isn’t publishing data on how often care-home residents are tested, or what inspection reports have found, Asagwara said.
“It is the vulnerable and marginalized communities that disproportionately suffer… who are paying the price for the government putting profit over people,” the MLA said.
Friesen said he’s optimistic Manitoba has the flexibility to get enough staff inside care homes.
“There isn’t a single province or territory that is saying they are out of the woods right now, when it comes to identifying the workforce they need to respond to a global pandemic,” he said.
The profit imperative
The greatest risk factor for COVID-19 reaching care homes — beyond widespread transmission in the surrounding community — is private ownership , according to Stall’s research.
He compared 190 outbreaks at Ontario care homes in the spring and found lengthier and deadlier outcomes in for-profit homes, particularly the ones owned by chains.
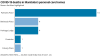
That bears out in Manitoba, where 80 per cent of care-home residents who died from COVID-19 lived in facilities run by Revera, a company with more than 500 senior-living residences in Canada, the U.S. and the United Kingdom.
Stall says chains buy older buildings, with rooms that house multiple residents. They often have outdated ventilation systems, a particular concern as research increasingly suggests the virus might be able to float in the air in concentrations large enough to infect people.

Parkview Place opened in 1964 and the 13-storey building has many shared rooms. A worker there tested positive in April, but the facility did not record another COVID-19 case until a full-blown outbreak began in mid-September.
Jackson said the nurses union has many more PPE complaints from privately owned facilities.
In Manitoba, about one-fifth of care-home beds are run by for-profit companies, compared with about 50 per cent in Ontario.
Friesen resisted comparing private and public ownership, arguing that what matters is upholding a standard of care and accountability for those who breach it.
“This is not an ideological issue and it should not be boiled down to some sort of false conversation about who is providing the care,” he said.
An inevitability?
The province has suggested deaths in personal care homes are inevitable, an idea that horrifies Stall.
“There is no jurisdiction in Canada in which there have not been deaths in personal-care homes,” Friesen told CBC a week ago.
“It is tragic, it is regrettable — but it is unavoidable, and to try to disclose somehow that that is not the case wouldn’t be honest,” he said.

Friesen told the Free Press he was expressing a concern about older people living in congregate settings.
Yet Stall said it’s an ageist viewpoint that ignores the success of countries such as Singapore and South Korea in stamping out COVID-19 from where the most vulnerable residents live.
B.C. ramped up infection controls and was able to limit care-home outbreaks early in the pandemic, he noted.
“I’m shocked that (Manitoba officials) just accepted this fatalistically, as an inevitable outcome, because it is not. We’ve seen in British Columbia that there are ways to do this differently, that can save lives, that should be saved,” Stall said.
“Having one of these outbreaks with (multiple) deaths is not an inevitability. If that’s the conclusion of having this, I think that’s a very tragic and sad statement, to be honest.”
Asagwara said a lack of preparation in the spring is leading to the growing horror unfolding each day in Winnipeg now.
“It didn’t have to be this way, which is what I think is the most devastating.”
dylan.robertson@freepress.mb.ca
With files from Danielle Da Silva and Michael Pereira
History
Updated on Friday, October 23, 2020 7:49 PM CDT: Fixes typo.