Logan’s legacy Parents of Humboldt Broncos player hope his organ donation continues inspiring others to give gift of life
Read this article for free:
or
Already have an account? Log in here »
To continue reading, please subscribe:
Monthly Digital Subscription
$0 for the first 4 weeks*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*No charge for 4 weeks then price increases to the regular rate of $19.00 plus GST every four weeks. Offer available to new and qualified returning subscribers only. Cancel any time.
Monthly Digital Subscription
$4.75/week*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*Billed as $19 plus GST every four weeks. Cancel any time.
To continue reading, please subscribe:
Add Free Press access to your Brandon Sun subscription for only an additional
$1 for the first 4 weeks*
*Your next subscription payment will increase by $1.00 and you will be charged $16.99 plus GST for four weeks. After four weeks, your payment will increase to $23.99 plus GST every four weeks.
Read unlimited articles for free today:
or
Already have an account? Log in here »
Hey there, time traveller!
This article was published 24/03/2022 (1357 days ago), so information in it may no longer be current.
We are only a few minutes into our Zoom call when Bernadine and Toby Boulet remind me there is still an infinite reservoir of tears to shed over the death of their son, Logan.
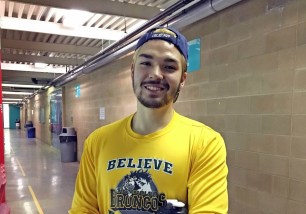
Logan was one of 16 members of the Humboldt Broncos junior hockey team that died following the horrific April 6, 2018, collision between the team bus and a semi-trailer in central Saskatchewan.

The family’s decision to donate six of his organs, a gift made possible by Logan’s decision to register as a donor, triggered a phenomenon that has since become known as the “Logan Boulet effect”: an immediate outpouring of support for Canada’s organ-donation program.
Following their emotional experience, Bernadine and Toby have become potent advocates for Green Shirt Day, an annual commemoration of the lives lost on that Saskatchewan highway that now serves as a national rallying cry for organ donation.
Facts about organ donations
Pre-pandemic, how many organ donations are performed in Canada and in Manitoba? In 2020, the last year for which complete statistics are available, 1,221 donors produced 2,622 organ donations in Canada. Manitoba only performs kidney transplants in the province; in 2020, 58 people received new kidneys.
How many people die each year waiting for transplants? In 2020, there were more than 4,100 people on transplant wait lists and 276 people died before they could get an organ. That included 13 Manitobans who died waiting for a kidney.
Pre-pandemic, how many organ donations are performed in Canada and in Manitoba? In 2020, the last year for which complete statistics are available, 1,221 donors produced 2,622 organ donations in Canada. Manitoba only performs kidney transplants in the province; in 2020, 58 people received new kidneys.
How many people die each year waiting for transplants? In 2020, there were more than 4,100 people on transplant wait lists and 276 people died before they could get an organ. That included 13 Manitobans who died waiting for a kidney.
Who can donate organs? Theoretically, anyone in an intensive care unit who falls into two categories: those who have suffered a catastrophic neurological injury and those who suffered a fatal cardiac event. In all instances, potential donors must have no brain activity and require a ventilator. Every patient that falls into those categories is “referred” to an organ-donation team for a consultation.
A little less than half the organ donations in Canada come from living donors; 87 per cent of those donate a kidney, while 13 per cent donate a lobe of liver.
Does everyone who falls into those two categories of ICU patients automatically become a donor? Although everyone is referred, only about 35-45 per cent of all referrals are approved by surviving family and go on to medical testing to see if any of their organs are fit for donation; only three per cent of all cases result in a viable donor.
If I register online to be an organ donor, does that mean I’ll become an actual organ donor? In Canada, as is the case in most other countries, even when someone has clearly indicated their wish to become an organ donor, the senior-most member of surviving family must still provide consent. If they say no, the donation process ends.
Are Canadians more likely to be organ donors than the citizens of other countries? Canadians donate 70.6 organs per one million residents, which is better than Australia (59) and the United Kingdom (57) but lagging behind the United States (120) and Spain (93.2). Of those countries, Canada has the highest rate of lung donors and living liver donors.
How many Canadians have pre-registered as organ donors? Even with a decline in actual organ transplants because of the pandemic, more than a million Canadians have registered as organ donors. Unfortunately, there are more than 21,000 people on organ-transplant wait lists across the country.
SOURCE: Canadian Blood Services
Friday night, the Boulets will make an emotional appearance at the Canada Life Centre just prior to the Winnipeg Jets game with the Columbus Blue Jackets to promote this year’s Green Shirt Day on April 7 (greenshirtday.ca). Their message is simple but powerful, and underlined by a grief that simply will not relent.
“We’re simply not going to let people forget about the Humboldt Broncos and the importance of organ donation,” Bernadine says. “We’ll go anywhere, speak anywhere. We don’t ask for money. Any money people donate goes to the cause.”
Bernadine pauses, her voice choked with emotion and tears welling up in her eyes. “We’re just not going to let people move on from this story.”
● ● ●
As many hockey families do in this country every winter, Bernadine and Toby Boulet were on the road in central Saskatchewan, nine hours and about 900 kilometres from their home in Lethbridge, all for a chance to see their son Logan play a Friday night playoff game against the Nipwawin Hawks.
They were about 15 minutes behind the team bus when they approached the intersection of highways 35 and 335 — known to locals as Armley Corner — and immediately saw a scene of utter devastation.

A semi hauling two trailers of peat moss blew through a stop sign right in front of the Broncos’ bus. It plowed into the first trailer, killing the bus driver and 13 of the passengers, and injuring 13. Two others, including Logan Boulet, died later in hospital.
As soon as they realized it was the Broncos’ bus, the Boulets tried to find Logan. Paramedics on scene informed them he had been airlifted to Saskatoon’s Royal University Hospital with a severe spinal cord injury.
On the drive to Saskatoon, Bernadine says, she and Toby immediately started “rationalizing what had happened.” Although they both knew Logan could be permanently disabled from his injuries, they were confident in that moment he would live.
Bernadine says she ran through a checklist of all the things they were going to have to do: modify their home in Lethbridge, find ways for Logan to pursue sports, maybe as a paralympian.
When they arrived at the hospital, however, it turned out things were much worse than they were first told.
Before they were allowed to see Logan, they met with the medical team that had been caring for him. It was then they learned that in addition to a severed spine, Logan had suffered a catastrophic brain-stem injury and was being kept alive on a ventilator. There was no brain activity, and Logan would never regain consciousness.
It was at that moment, under the crushing weight of grief, that Bernadine blurted out a single question.
“Can we donate Logan’s organs?”

It was a stunning moment for everyone in the room. Rarely, if ever, do families of fatally injured Canadians raise the issue of organ donation on their own. Equally stunning was that Bernadine had been unaware of an important fact: several weeks earlier, just before his 18th birthday, Logan had already told his father he wanted to donate his organs.
“Everyone just stopped and looked at us,” Bernadine recalls of that day. “All I could think of was that Logan is young, fit and healthy, and someone could use his organs and have a life. Logan could live on and help other people.”
Toby still shakes his head at the moment of revelation.
He says Logan had been particularly moved by the loss of his friend and conditioning coach Ric Suggitt, who died suddenly in 2017 from a brain hemorrhage. Although he had not registered as an organ donor, his wife Jennifer said she and her husband had discussed it and it was definitely something he wanted.
“Logan talked about Ric a lot and he told me that he wanted to be an organ donor,” Toby says. “He loved Ric and the fact that Ric was able to help so many people with his organs, it really made an impression with Logan. Bernie had no idea of what Logan wanted until that moment. But Logan had told me he was going to be an organ donor. It made so much sense in that moment.”
No one could have predicted the impact this one decision would have on the nation’s attitudes towards organ donation.
The Humboldt Bronco tragedy was the biggest story in the country for weeks. And once news media began to publicize Logan’s organ donations, it did not take long for the “Logan Boulet effect” to manifest.

In the weekend following Logan’s death, many provincial organ-donation programs noticed a significant uptick in online registrations. The Kidney Foundation of Canada estimated that in the two months following the crash, 150,000 Canadians registered as organ and tissue donors.
Although the surge in support for organ donations was welcomed, much of that momentum was erased by the pandemic. Although the final numbers for 2021 are not in yet, it would seem the enormous burden COVID-19 placed on the health-care system has significantly cut down on transplant activity.
“We’re still trying to get a fix on how bad things are, but we’d have to be naive not to acknowledge that the pandemic had a negative effect on transplants,” says Dr. Owen Mooney, medical director of Transplant Manitoba’s Gift of Life Program.
The pandemic presented a number of significant problems, Mooney adds. Operating rooms were closed, in part because of the threat of COVID-19 infection and in part because OR nurses and other staff were transferred to pandemic units. Transplant teams, which typically transport patients and organs across the country, were limited by pandemic travel restrictions.
The system was under so much stress, Mooney says, that patients in intensive care units who were theoretically eligible to become donors — on life support and absent of any brain activity — were not being referred to the transplant team for consultation.
Canadian Blood Services, which tracks most of the data about organ donations and transplants, reported that living organ donors declined by 30 per cent in 2020, the first full year of the pandemic. And deceased donors also dropped by about 21 per cent.
Mooney says it’s not clear yet why referrals and donations are down by so much. However, with a massive reassignment of OR and ICU staff, it was also impossible to undertake the complex work of obtaining the organs and getting them where they were most needed.
At the same time, Mooney says, the pandemic also unearthed a lot of deep-seated concern about the health-care system that was triggered by the pandemic.
“Organ donation has always been a difficult issue to navigate because of the conspiracy theories that we have to deal with,” Mooney says. “Some people still think that physicians will not do everything they can to save a patient so they can be organ donors. Or that somehow organs are being sold.
“Some of the issues that arise create a real quagmire for organ donation. We need to be very strong advocates to overcome some of the misconceptions and misinformation out there.”
Largely to address these concerns, most jurisdictions including Manitoba have a strict policy that prevents physicians who are treating someone’s injuries from being involved in any discussion with a patient’s family about organ donation. Once it has been determined a patient has no brain activity and will not recover, the family are told about “end-of-life options” that include orders to withdraw life-sustaining treatment. It is at that point organ donation is mentioned as one of those end-of-life options.
If the family consents, they are then referred to a separate transplant team to discuss the process by which a donation can be made. This is a key moment: even if the patient has already registered to be an organ donor, the transplant team must obtain explicit consent from the surviving family. This is not an insignificant hurdle and explains in part why more people die each year on transplant waiting lists than consent to be organ donors.
In 2020, of the 362 total referrals that were made involving Manitoba ICU patients, only 27 families consented to be donors. Out of that group, 20 were found to be medically viable as donors.
That same year, the number of patients on transplant waiting lists who died was 26.
“Our families are made aware that organ donation is an option and if they want to talk to someone about what’s involved, we put them in touch with one of our teams,” Mooney says. “For families, this is perhaps the worst moment of their lives and a lot of thought has to go into a decision (to donate an organ).”
● ● ●
Mark Miles was staffing a Canadian Transplant Association information desk at a Winnipeg mall when a stranger came up to him and pointed an accusing finger.
“You can’t do that!” the stranger said angrily. “You’re just trying to harvest people’s organs!” Miles, a heart transplant recipient, tried to explain that organ donation is never done against anyone’s wishes. The stranger was undeterred, convinced that physicians actually withhold life-sustaining treatment to generate more organ donations.

“That is one of the biggest problems we face, for sure,” says Miles, principal of Marymound School in Winnipeg and provincial director of the Canadian Transplant Association. “It’s all of the misinformation and misconceptions people have about what organ donation is all about. They actually think physicians are pushing people to their deaths so that they can get their organs.”
Those misconceptions are particularly frustrating given that, in so many ways, organ donation has come a long way.
Gone are the flimsy paper consent forms on the back of driver’s licences. Now, the preferred method of registering is an online portal: signupforlife.ca. At the same time, advances in medical science allow a broader array of organs to be donated and a much higher rate of success for recipients.

And yet, the issue of organ donation is still largely mired in very traditional politics and ideology.
Governments have become masterful at turning a deaf ear to the demands of advocates for modernized laws that would require people to opt out — rather than opt in — to organ donation.
In Manitoba, the Law Reform Commission provided a report to the Progressive Conservative government that serves as a blueprint for the establishment of an opt-out organ-donation program, where everyone is presumed to be a donor unless someone asks specifically to be excluded. Controversial for many, opt-out programs are viewed by advocates as the next step forward in the advancement of organ donation.
Not surprisingly, the PC government has not formally responded to the report.
The evidence in most jurisdictions is that opt-out protocols and advance registration help ensure not only a larger number of donor referrals, but also a certain clarity about your intentions, Miles says. However, in Canada and in fact in most countries around the world, surviving family are still allowed to veto an organ donation even if someone has formally registered as a donor, he adds.
Currently among the provinces, only Nova Scotia has a formal opt-out organ donation system. However, even there, family consent is required to move the process forward.
Most organ-transplant advocates support the notion of family consent but believe that many of those skeptical families would be more at ease if people registered as donors and presumed consent were the law of the land.
“I don’t think government has the stomach for (those changes) and that’s what I find so frustrating,” Miles says. “But what we’re talking about here really is a gift of life. And I think most people, when you explain it to them, would support that.”
dan.lett@winnipegfreepress.com

Born and raised in and around Toronto, Dan Lett came to Winnipeg in 1986, less than a year out of journalism school with a lifelong dream to be a newspaper reporter.
Our newsroom depends on a growing audience of readers to power our journalism. If you are not a paid reader, please consider becoming a subscriber.
Our newsroom depends on its audience of readers to power our journalism. Thank you for your support.