Pro-truth A Winnipeg doctor breaks down what happens before, during and after the termination of a pregnancy
Read this article for free:
or
Already have an account? Log in here »
To continue reading, please subscribe:
Monthly Digital Subscription
$0 for the first 4 weeks*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*No charge for 4 weeks then price increases to the regular rate of $19.00 plus GST every four weeks. Offer available to new and qualified returning subscribers only. Cancel any time.
Monthly Digital Subscription
$4.75/week*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*Billed as $19 plus GST every four weeks. Cancel any time.
To continue reading, please subscribe:
Add Free Press access to your Brandon Sun subscription for only an additional
$1 for the first 4 weeks*
*Your next subscription payment will increase by $1.00 and you will be charged $16.99 plus GST for four weeks. After four weeks, your payment will increase to $23.99 plus GST every four weeks.
Read unlimited articles for free today:
or
Already have an account? Log in here »
Hey there, time traveller!
This article was published 28/05/2019 (2386 days ago), so information in it may no longer be current.
Jillian Groening was 25 when she got a phone call she never wanted to get. It was her doctor, informing her she was pregnant.
“I’m someone who, as of right now, is pretty confident I don’t want kids,” says Groening, now 29. “I love children and I love my pals who have kids, but it’s not something I’ve ever seen in my future.”

She was in a relationship and in between birth-control methods at the time. “Having a kid at that time was not an option, not at all. Getting that phone call from my doctor about being pregnant was the worst,” she says.
For Groening, finding Women’s Health Clinic was like locating a lighthouse at sea. WHC, along with Health Sciences Centre, are the two places one can obtain abortion care in Winnipeg.
“Being able to talk to a counsellor who was really knowledgeable and validating and become informed of options was fantastic,” she says. “It’s so pro-choice, no matter what route you want to take.” Groening was so moved by the care she received when she got her abortion, she became an abortion counsellor herself at WHC.
Abortion stories like Groening’s are not uncommon. In fact, they are more common than people may realize. But, for a legal medical procedure that’s endlessly debated and politicized, the realities of abortion remain largely hidden from view.
There is an intense focus on abortion rights thanks to news out of the United States, where several states are rushing to pass aggressive restrictions on the procedure in a systematic attempt to overturn Roe v. Wade, the landmark 1973 U.S. Supreme Court ruling that protects a woman’s privacy rights, allowing her to choose to have an abortion. The unstable landscape of reproductive rights south of the border is stirring up anxiety in Canada as well as renewing conversations about the inequities in access that exist here.
Even those attempting to make laws on the procedure… lack basic understanding of how pregnancy and abortion work
Whenever abortion re-enters the news cycle, the amount of ignorance, misinformation and fear-mongering that exists is brought into stark relief. Even those attempting to make laws on the procedure — such as the Ohio Republican who laughably suggested an ectopic pregnancy, in which an embryo attaches outside the uterus, can be relocated to the uterus — lack basic understanding of how pregnancy and abortion work.
“People need to realize abortion is part of reproductive rights and health,” Groening says. “We need more education in that realm.”
To that end, the Free Press sat down with Dr. Nadin Gilroy, who is an abortion provider as well as the medical director of the abortion program at Women’s Health Clinic, to get the facts on abortion.
Who gets an abortion?

The short answer is, any person who can get pregnant and does not want to be pregnant. The reasons for needing abortion care are personal and varied.
“We generally think of abortion as women who, for whatever reason, understand that this is not a good time for them to carry a pregnancy to term and have a child,” Gilroy says. “However, there are also women who find themselves in situations where they find that there are issues or anomalies with the fetus that are not compatible with life or pose a danger to the fetus and the mother.”
Gilroy points out that those kinds of terminations are also done away with when laws are changed or the procedure is made inaccessible.
‘A lot of the women I see already have children. They don’t make these decisions in isolation, and they don’t make them frivolously. They think this through very carefully’
— Dr. Nadin Gilroy
“And those issues are potentially discovered in later stages of pregnancy,” she says. “To demonize families who find themselves in these incredibly difficult situations where they have to make difficult decisions around their health and change course at a time when they were expecting something different is absolutely cruel.”
The age range of women Gilroy sees is anywhere between 15 and 45, and sometimes older than that.
“A lot of the women I see already have children,” she says. “They don’t make these decisions in isolation, and they don’t make them frivolously. They think this through very carefully.
“I don’t see how men can absolve themselves from the picture and the discussion because I know for a fact a lot of them are involved in these conversations with their partners and the decision is made together,” she adds. “I sometimes feel it would be helpful if they started to speak up a little louder, too.”
What happens before an abortion?
You pee on a stick and two blue lines appear, or you get a call from the doctor. The pregnancy test is positive. Then what?
“If a woman finds herself pregnant and decides she wants an abortion, she would call one of two numbers: the hospital intake number or the Women’s Health Clinic intake number. In that first encounter, they will ask her certain questions about how far along she might be and, based on that, she’ll either get booked with us in our program or referred to the hospital and their program. Then she gets an appointment.”
For the purposes of this article, we will focus on the process at Women’s Health Clinic.
When a client arrives at the appointment, a medical history is taken, and then an ultrasound is performed to see how far along the pregnancy is. “Women at the Women’s Health Clinic who are nine weeks pregnant or under have the option of having a medication abortion or a surgical abortion,” Gilroy says. “Over nine weeks it would have to be a surgical abortion.”

In Manitoba, the highest gestational age in terms of termination is 19 weeks and six days at the hospital; at the Women’s Health Clinic, it’s 15 weeks and six days. “The majority of women we see are between six and 10 weeks,” Gilroy says.
In the U.S., several states have passed so-called heartbeat bills, which would ban abortion at six weeks, or once a “fetal heartbeat” can be detected. But “heartbeat” is not a medically accurate term for what is detected at six weeks, Gilroy says.
“They’re talking about detecting heart motion on an ultrasound,” she says. “People, when they hear that, imagine a body and vascular system like yours and mine. That’s not happening. When a woman goes through with a pregnancy, generally speaking, it’s rare you’d detect heartbeat sound with a doppler at around eight weeks. It’s much more common around 10 or 11 weeks.”
Once the type of abortion has been determined, the client will then meet with a counsellor, who is there to make sure this is indeed the client’s choice, and that there’s been no outside pressure or coercion. From there, they discuss the client’s health in general as well as any concerns about the procedure. The counsellors will also go over a birth-control plan and methods with the patient, as well as the consent to the procedure.
There is no cost to have a medical or surgical abortion at Women’s Health Clinic so long as one has a Manitoba Health Card or coverage from another province.
What happens during a medication abortion?
First, an IV is started and blood is drawn.

“The bloodwork that’s done checks for the blood type and Rh status, which is an important piece in pregnancy and some women are Rh negative. They are also offered a check for any STIs, which is up to them. For the medication abortion clients, a beta hCG is sent off. That’s the pregnancy hormone, basically, that can be measured in the blood,” Gilroy says.
“If they have chosen a medication abortion, they are seen by the physician who reviews the medical history and makes sure there’s no contraindication to a medication abortion. We review the counselling forms and ultrasound. If everything looks like it’s within guidelines and best practices, we explain the medication.”
What is commonly referred to as the “abortion pill” is really two oral medications: mifepristone and misoprostol. These medications are not the same as Plan B, or “the morning-after pill,” which attempts to prevent the implantation of a fertilized egg.
“We go over how to take them, what to expect, what would be things to be concerned about,” Gilroy says. Mifepristone is taken at the clinic, misoprostol is taken at home. Bleeding is expected, excessive bleeding is not. The guidelines for excessive bleeding are filling two maxi pads — “those fat ones no one wants to wear” — in one hour, for two hours in a row, or passing a clot larger than the size of a lemon.

Ibuprofen is recommended for pain management. Aspirin may increase bleeding.
Clients will leave with information about the birth-control plan they’ve chosen, usually with a sample or prescription, as well as a follow-up bloodwork requisition. “In order to determine (the medication abortion) was successful, we do two things: one is that we repeat the beta hCG five days after taking the mifepristone and we compare the first level drawn when they were with us to the level that was drawn later,” Gilroy says. “We know it should have dropped by more than 80 per cent.”
The second part is a follow-up, by phone or in person, where a nurse goes through a set of questions and women are able to share their experience.
The regimen on mifepristone and misoprostol, known under the brand name Mifegymiso, has been heralded as a game-changer when it comes to improving access to abortion care because they can be taken remotely. But barriers remain, including, most significantly, cost. The drug is only available for free at the three clinics that provide medication and surgical abortions in Manitoba — WHC and HSC in Winnipeg, and the Brandon Regional Health Centre. Those living outside of those communities have to pay about $350.
What happens during a surgical abortion?

The first part of the process is the same as a medication abortion. Patients will change into a wraparound skirt and will move into the waiting room.
In the procedure room, the client is introduced to a nurse who is there to support the patient, a medical assistant who supports the physician, and the physician.
“At this point, the physician would have reviewed her chart, that there’s no concerns, that the choice of birth control doesn’t pose issues with medical history, and that the ultrasound was good and showed what we needed to see to proceed. If all of that is fine, we have a brief conversation with the patient reviewing consent again, checking in one more time, reviewing the birth-control plan.”

The nurse will get the client into position. The client will receive midazolam, a sedative, and fentanyl, a painkiller, for what’s called a “procedural sedation,” which doesn’t put a person out completely. Some women choose not to use medication at all.
The physician will conduct a bi-manual internal exam, similar to a Pap test, which is done to assess the position and size of the uterus, and confirm information from the ultrasound.
“There’s a nice picture above the bed women lay on of the Three Sisters, the three massive spruce trees in B.C.,” Gilroy says. “Those trees generally start to move once the medication starts to work, but it’s a feeling of being in a forest rather than in a procedure room.”
The abortion is performed under sterile conditions. A speculum is inserted and a swab is taken to test for chlamydia and gonorrhea as well as for bacterial vaginosis, an overgrowth of bacteria in the vagina that’s common in pregnancy. If BV is present, it’s treated with antibiotics to make sure no infection is transferred to the uterus.
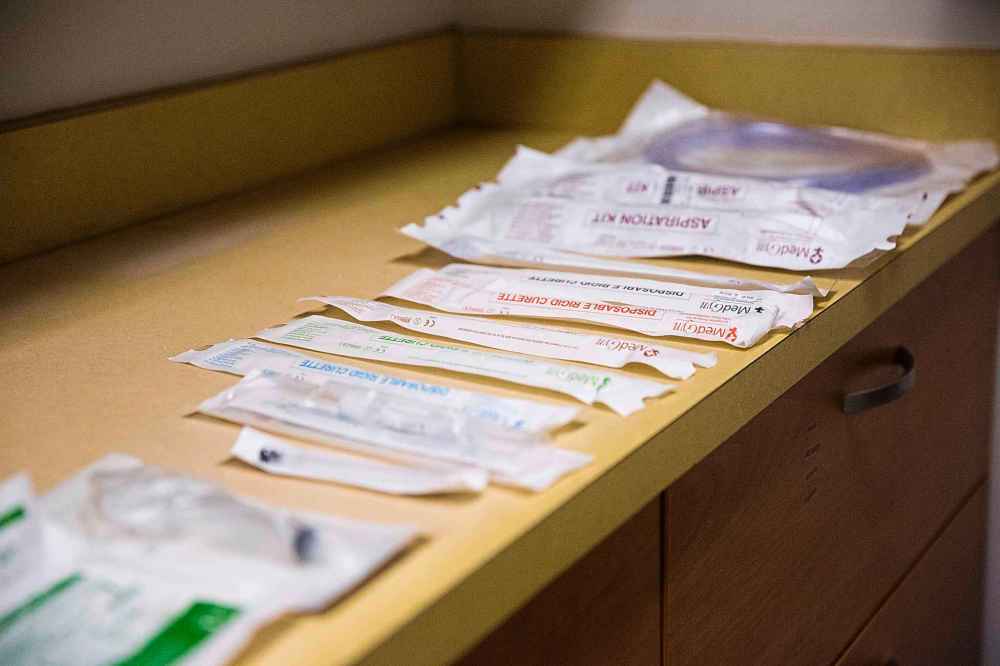
Local freezing is applied around the cervix, which is then dilated. The physician uses an instrument called a manual vacuum aspirator — a small tube and a syringe that are attached to each other — to empty the contents of the uterus. “For women of slightly higher gestational age, a machine is used.” The procedure itself takes two to three minutes.
Clients will then move to the post-op area, where their heart rate, blood pressure and saturation are monitored. Usually within 15 and 20 minutes, they’ll get up and go to the washroom and report on bleeding, if any. As with the medication abortion, patients will receive information on what constitutes excessive bleeding of infection. They are advised not to insert anything into the vagina for seven days, and not to soak in hot tubs, which could lead to infection. They will need a ride home.
And as with the medication abortion, clients will be provided with their birth-control choice and instructions, including when to start it. If a client chooses an intrauterine device (IUD), the physician can do the insertion right after the abortion procedure is done while they are frozen so they don’t have to come back to the clinic.
How can I expect to feel emotionally after an abortion?

It’s typical to feel a range of emotions post-abortion. There’s no “right” way to feel.
Groening, like many women, reported feeling an overwhelming sense of relief after her abortion.
“After a month of worry and stress and anxiety about having something I didn’t want… oh my gosh, I can’t imagine continuing a pregnancy to term that you didn’t want,” she says. “Six weeks was stressful enough.”
“I think the emotional work women do to come to the decision, if there is that piece, is usually done by the time they’ve made their decision,” Gilroy says. “Most women are hugely relieved and thankful they have this available to them in a safe environment.”
Women’s Health Clinic does provide post-abortion counselling if needed.
How can we challenge the stigma surrounding abortion?
“One of the pieces is not to hide it, to talk about it,” Gilroy says. “To use the word ‘abortion’ without whispering or hiding it behind your hand. And to challenge our people in our lives, including the men in our lives, to understand that it’s very common for a woman to have had an abortion and likely they have someone in their lives who has had one, and to be curious about that and to ask what that meant, because most will tell you it meant a great deal to them in terms of where they’re at now in their lives.
”And to not let go of reminding our politicians that they have a responsibility to ensure all health care is available to all of us. Stigma happens because we hide things. The only way to counteract that is to be upfront and loud about it.”‘One of the pieces is not to hide it, to talk about it. To use the word “abortion” without whispering or hiding it behind your hand’
— Dr. Nadin Gilroy
“Once you start talking to friends and other women in your life, you realize so many of them have that experience in their past,” Groening says. “Some feel more open about talking about it than others and that’s OK, too. It’s such a normal part of having a uterus.”
jen.zoratti@freepress.mb.ca
Twitter: @JenZoratti







Jen Zoratti is a Winnipeg Free Press columnist and author of the newsletter, NEXT, a weekly look towards a post-pandemic future.
Our newsroom depends on a growing audience of readers to power our journalism. If you are not a paid reader, please consider becoming a subscriber.
Our newsroom depends on its audience of readers to power our journalism. Thank you for your support.
History
Updated on Tuesday, May 28, 2019 8:02 PM CDT: Fixes typo.
Updated on Tuesday, May 28, 2019 8:03 PM CDT: Fixes typo.



















