Better planning means better health care
Advertisement
Read this article for free:
or
Already have an account? Log in here »
To continue reading, please subscribe:
Monthly Digital Subscription
$0 for the first 4 weeks*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*No charge for 4 weeks then price increases to the regular rate of $19.00 plus GST every four weeks. Offer available to new and qualified returning subscribers only. Cancel any time.
Monthly Digital Subscription
$4.75/week*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*Billed as $19 plus GST every four weeks. Cancel any time.
To continue reading, please subscribe:
Add Free Press access to your Brandon Sun subscription for only an additional
$1 for the first 4 weeks*
*Your next subscription payment will increase by $1.00 and you will be charged $16.99 plus GST for four weeks. After four weeks, your payment will increase to $23.99 plus GST every four weeks.
Read unlimited articles for free today:
or
Already have an account? Log in here »
Hey there, time traveller!
This article was published 07/04/2017 (3174 days ago), so information in it may no longer be current.
On Friday, the Winnipeg Regional Health Authority announced a plan to heal the health-care system, making fundamental and necessary changes that reduce wait times, promote access to services and ensure the sustainability of the system itself. Manitobans have every reason, today, to feel positively about that plan.
My colleagues and I spent 2016 studying the needs of patients in Manitoba and attending hundreds of meetings with community representatives, Regional Health Authority leadership and staff, unions and associations, indigenous organizations, clinical leaders in all major specialties across the province and other important stakeholders, all aimed at identifying major opportunities to improve care, enhance prevention and make the system more financially sustainable.
While stakeholder perspectives varied, their goals were shared: build a system aligned with the needs of those it serves, structured in a way that makes sense, and built on a commitment to sustain it for generations to come. Health-care systems and planning must break away from the mindset that “more is better” — evidence is compelling that this is simply untrue. Accessibility, quality and equity are founded in evidence-based planning premised on need and new models of collaborative care.
Recently, each Regional Health Authority developed clinical plans that reflect priority needs and health service delivery models consistent with the provincial plan. Some included redefining the role of hospitals to better meet patient need, increasing home care capacity, enhancing collaborative care models that use the full scope of practice for all types of providers, and strengthening the care of older adults at more elder-friendly facilities. The recently released WRHA Healing Our Health System Plan reflects these approaches and is an important step in the right direction.
The clinical and preventive services plan is an example of how “more” can be replaced with “better” — all to the benefit of patients. Acute services had become diluted in the city, and non-acute services, such has home care, chronic care, and long-term care, more difficult to access in a timely fashion.
A transition to grouping emergency medicine, critical care and related medical and surgical services from six sites to three in Winnipeg will give these hospitals a critical mass to improve access and efficiency, all significant factors in improving quality for patients. As well, the remaining hospitals in the city, in parallel, will transition to improved and expanded convalescent and rehabilitation services, with two providing urgent care for those patients not requiring emergency services of the greatest intensity.
Any change can be difficult, especially when it relates to something as important as health care; still, a failure to change will diminish the overall impact of the clinical and preventive services planning and impair the ability to meet patients’ needs in Manitoba. Further, the plan must transform the sectors of acute care, mental health and addictions, care of indigenous peoples, palliative care, care of older adults, home care, and primary care. These actions alone will distinguish the province as a leader in care and outcomes. Combined with the other dimensions in the plan, there is a real opportunity to redefine healthcare, boldly, in an evidence-based and cost-efficient manner.
Health-care systems that are unplanned or outdated rarely, if ever, reach this potential; the level of commitment begins with high political office and senior management, and extends through an interdependent network of management and staff, characterized by mutual respect and a collective commitment to integrated, collaborative care.
Successful planning provides better services for patients and their families, and opportunities to address inequities. In the long term, it requires commitment across the system, belief in the values of the system, and the imperative for change that maintains patients at the centre of that system.
All of the requirements for the plan to succeed are in place in Manitoba, in the context of care driven by a belief in the values of a safe and sustainable health-care system that is equitable and accessible. Doing things differently and better will reflect new models of collaborative care, where all providers are working at the top of their scopes of practice.
The plan is the beginning of a journey, not the end. The beliefs and values that underpin it can be reduced to a single question, “If it isn’t being done for the patient, why is it being done?”
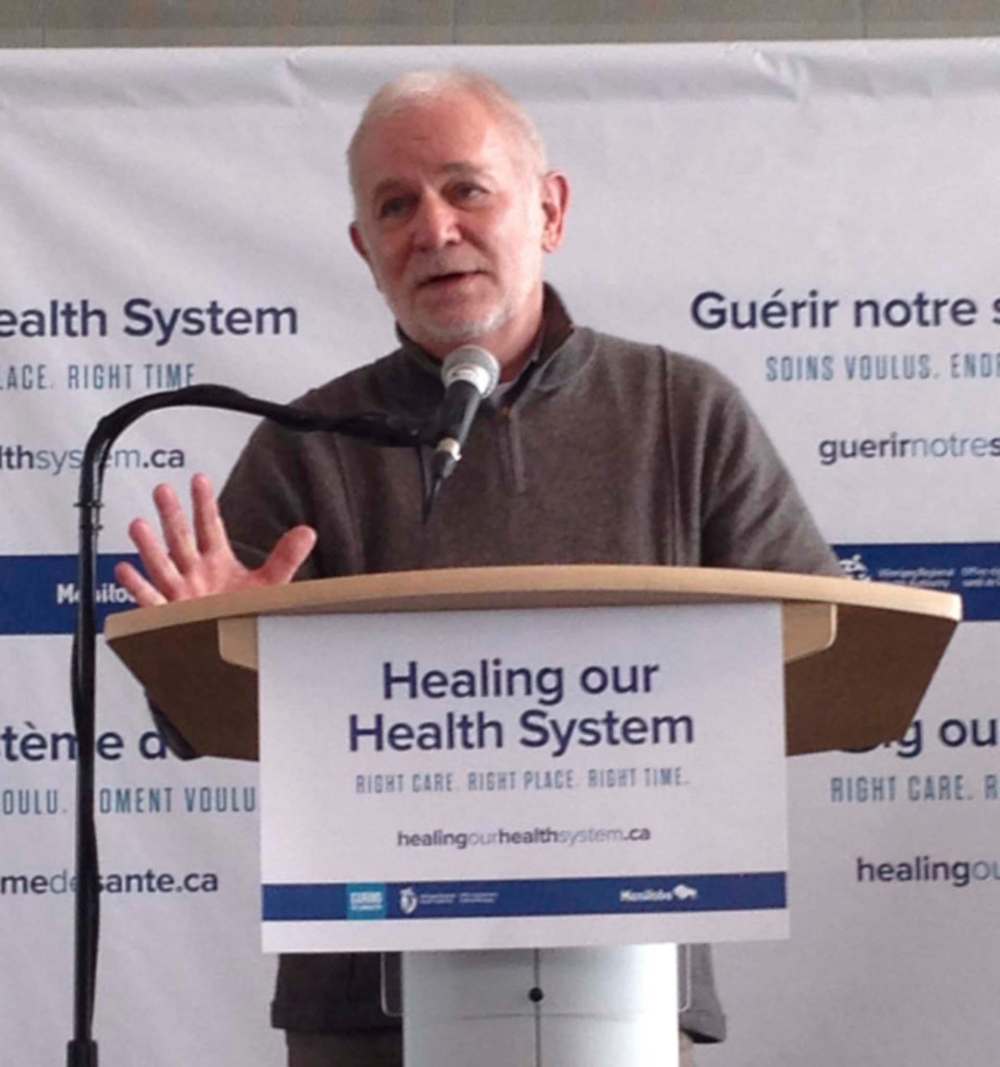
David Peachey is a physician and the principal of Health Intelligence Inc. He was the lead consultant in the development of the clinical and preventive services plan for Manitoba.



