At death’s locked door Anguished patients, families lose faith in health system when right to die takes back seat to care facility's religious beliefs
Read this article for free:
or
Already have an account? Log in here »
To continue reading, please subscribe:
Monthly Digital Subscription
$0 for the first 4 weeks*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*No charge for 4 weeks then price increases to the regular rate of $19.00 plus GST every four weeks. Offer available to new and qualified returning subscribers only. Cancel any time.
Monthly Digital Subscription
$4.75/week*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*Billed as $19 plus GST every four weeks. Cancel any time.
To continue reading, please subscribe:
Add Free Press access to your Brandon Sun subscription for only an additional
$1 for the first 4 weeks*
*Your next subscription payment will increase by $1.00 and you will be charged $16.99 plus GST for four weeks. After four weeks, your payment will increase to $23.99 plus GST every four weeks.
Read unlimited articles for free today:
or
Already have an account? Log in here »
Hey there, time traveller!
This article was published 24/02/2018 (2849 days ago), so information in it may no longer be current.
One Friday last December, Karin Woods asked the nurse at St. Boniface Hospital to sedate her husband so he would barely feel his own death. She asked for more sedatives repeatedly over the weekend.
George Woods had pleural mesothelioma from workplace asbestos exposure and she didn’t want him to die horribly — he didn’t want to die horribly — feeling as if he was suffocating right up until the very moment he stopped breathing.
On Monday, Dec. 11, he died. He was 77 years old.
“Fortunately, he died a peaceful death,” Woods says, “but that’s not the point.”
The point, she says, is that he knew his death was coming and he knew it would likely be painful, so he wanted to invoke his right to medical assistance in dying in hopes of making an already agonizing process less so. The provincial Medical Assistance in Dying (MAID) team had already assessed Woods once at home by the time extreme pain forced him into the hospital. He asked not to be taken to St. Boniface because he knew the Catholic-based facility doesn’t allow assisted deaths on site, but Woods says that was where the couple was told a bed was available, so that was where they had to go.

In the end, staff in the hospital’s palliative unit and the members of the MAID team determined Woods too frail to be transferred without sedatives, which would render him unable to provide the consent necessary for an assisted death, making the transfer futile. So Woods leaned in to her husband’s side, asking the nurses for more drugs that would pull him under, and hoped death would come quick and painless.
“Just give him more sedatives,” she implored.
Of the 63 people who died with medical assistance in Manitoba last year, 10 — roughly 16 per cent — had to be transferred out of faith-based facilities. Of the 11 people who died with assistance in January, two required transfers.
The WRHA’s protocol for assisted dying transfers
1. An individual at an abstaining, faith-based facility tells someone they either wish to seek an assisted death or want to learn more about it. At this point, they are identified as possibly needing a transfer.
- An individual at an abstaining, faith-based facility tells someone they either wish to seek an assisted death or want to learn more about it. At this point, they are identified as possibly needing a transfer. The MAID team should be involved, as should the site’s medical director or director of care, the attending physician, and the head of the site’s palliative program if necessary.
- Before the MAID team meets with an individual, they must tell the facility’s operator in advance of that first discussion to make sure everyone is aware of timing and possible transfer needs.
- After the first meeting, the MAID team will tell the facility’s operator whether the individual is eligible for MAID.
- If the individual has been approved, he or she will then tell the team that they want to move forward, at which point the team will inform the site’s operators that they plan to have a second eligibility meeting. At this stage, plans for a transfer will begin.
- If the individual is approved following the second meeting and still wishes to have an assisted death, the abstaining facility will develop a plan with the facility where the individual will be transferred. That plan will include “a determination of the required resources to safely transport the patient,” as well as “a determination of whether the receiving facility is able to meet the level of care required to support the individual during admission, through and until the provision of MAID.” Both the operator of the abstaining facility and the receiving facility need to agree the patient is medically stable if he or she is to be transfered.
- The patient is then told about the plan for a transfer.
- The MAID team then informs the operator of the abstaining facility and the receiving facility about how the second assessment went. The transfer plans are modified if necessary and then finalized.
- When the individual has picked his date to die, the MAID team will then inform the operator of the abstaining facility to allow the operator to perform “a final assessment of care needs and transfer plan is updated.
- The individual is then transported to the new facility with “appropriate support persons.”
- At this point, the abstaining facility will either be told that the patient has died or that he or she will be returning to them because either they are no longer eligible for MAID or have chosen, for whatever reason, not to go through with it.
Details of bungled transfers are starting to filter out elsewhere across the country. There is the mismanaged incident that prompted Providence Healthcare in British Columbia to apologize to one of its hospitals last May for “a foreseeable and preventable issue,” and then there is the wheelchair-bound man with multiple sclerosis in Vancouver whose catheter bag split open during a taxi transfer.
Three years after the Supreme Court struck down Canada’s ban on physician-assisted dying and nearly two years after the federal assisted dying law received royal assent, transfers have become a contentious battleground in the fight to reconcile equitable access with the rights of conscientious objectors.
● ● ●
When it became apparent the story of Cheppudira Gopalkrishna, whose request to die was tied up for months, was going to become public, the Winnipeg Regional Health Authority and Misericordia Health Centre (MHC) found themselves in a rare disagreement.
Gopalkrishna, an 87-year-old retired schoolteacher, has a form of ALS. He struggles with his memory. He’s lonely. His most fervent wish is to die and he hadn’t, as of that moment last fall, been able to connect with the people who could assess him and deem him eligible.

A story about his case will likely run “regardless of whether you comment or not,” wrote the health minister’s spokeswoman Amy McGuinness in an Oct. 22 email to Misericordia spokeswoman Heidi Klaschka, “it’s important that MHC is in the story.”
Klaschka, who had been waffling on an official statement due to privacy issues according to emails obtained through a freedom of information request, had a statement for the minister’s office to review within the hour.
In one bolded line, she made it clear the hospital felt the fault was not theirs: “Misericordia does not control the length of time it takes for the MAID team to be in contact with the patient.”
That the WRHA would flat out contradict Misericordia’s version of events became apparent days later when its then-spokeswoman Anne Bennett fired off the MAID team’s version of events to reporters without first running it past Misericordia. The major facts under dispute: that Misericordia staff not only provided Gopalkrishna with contact information for the team when he first asked on May 1, 2017, but that they also told the team about his request (the MAID team says that’s not the case). Also, whether he was physically able to connect with the team on his own (they say no, the hospital says yes).
“Would have appreciated seeing this in advance of you sending,” Klaschka wrote.
Within an hour, the issue had been elevated to Misericordia’s then-CEO Rosie Jacuzzi, who wrote to the WRHA’s chief health operations officer and asked for a retraction.
“This should be about the patient and not about faith-based facilities as we have a process that provides access to patient(s) inquiring or needing access to (the) MAID assessment process,” she wrote.
By the time Gopalkrishna’s story went public Oct. 26, the region and its faith-based facility had settled on their narrative. Jacuzzi wrote to Klaschka that when the WRHA’s CEO Réal Cloutier spoke to reporters he would emphasize it was the hospital’s first assisted-dying request, a learning experience.

“He is trying to put all of us in the same boat and wants a united front,” she wrote.
At the Thursday press conference, Health Minister Kelvin Goertzen called the case “troubling,” while Cloutier stuck with the agreed upon approach: “Obviously, we need to do much, much better.”
Gopalkrishna was transferred out, assessed and transferred back to Misericordia after the MAID team deemed him not yet eligible for the procedure. Health authority leadership began a months-long process to try to figure out where communication had gone wrong and how similar situations could be avoided in the future.
“You learn from these things,” Cloutier said in a recent interview.
“The timelines were tight. People were trying to gather information and respond and sometimes there was a little bit of a lack of clarity around the policy and procedures, which we’ve now cleaned up.”
On Dec. 19, following an extensive consultation, the WRHA board approved a new MAID policy, including proper procedures for transferring patients out of faith-based facilities. Individual facility policies were due Feb. 15 and expected to be sent off to Manitoba Health shortly thereafter.
“We’re in a much better place today,” Cloutier said.
And yet, Cory Ruf of Dying with Dignity Canada notes the regional policy contains one stipulation that underscores why people can still be left without the care for which they’re eligible. It states that every facility policy must make it clear that a person may not be able to access MAID if they are deemed “too ill or frail to be transferred.”
So you have George Woods, in the process of being assessed for medical assistance in dying when he has to be hospitalized for pain and has no say in where he is taken for treatment. Because its St. Boniface, his ability to access MAID becomes less certain.
“Even if St. Boniface Hospital and the WRHA and other bodies (such as Misericordia) are working to streamline their communication,” Ruf says, “it doesn’t eliminate the risk of a patient’s rights being denied unfairly.”
● ● ●

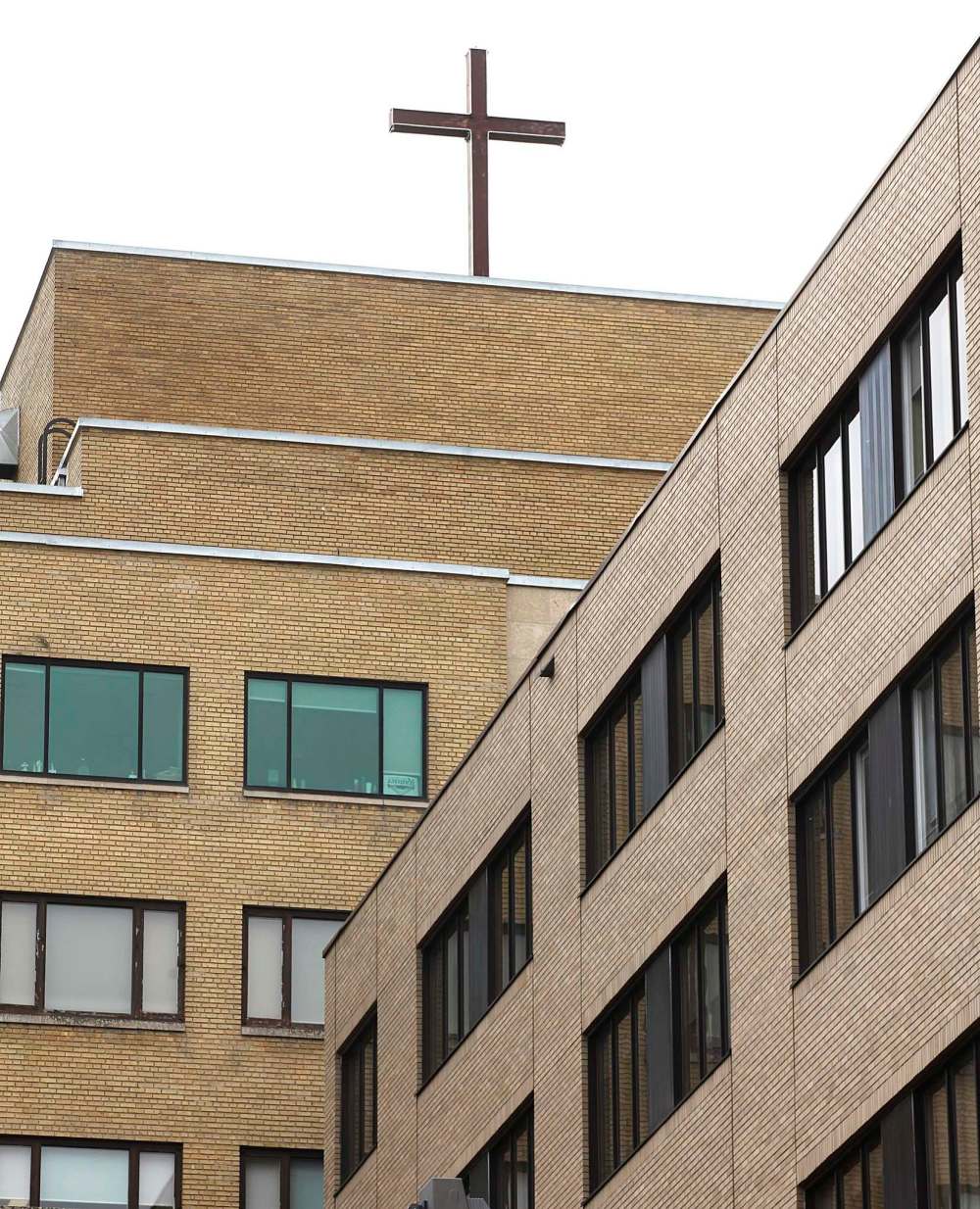
When St. Boniface opened its doors in 1871 with just four beds, it was the Grey Nuns who welcomed the first patients. More than a century later, the Prairies have evolved, but the hospitals the clergy built remain.
There is an expectation, says Brendan Leier, a clinical ethicist with Alberta Health Services, that these facilities at least align with Canadian constitutional values. You hold respect for their legacy in one hand, he says, while also being attentive to the people they care for now.
“Oftentimes the devil’s in the details,” Leier says.
Meaning, you can accept clearly that it’s not OK for them to be biased with whom they provide healthcare to, while at the same time struggling with some of the greyer considerations: “Should your hospital have to take the cross down in your room if it’s the only hospital in town and that makes you uncomfortable?”
People are still grappling with those questions.
What has clearly changed, Leier says, is the faith of the people staffing faith-based facilities.
“The majority of people working inside of these institutions are secular people,” he says, “or at least don’t share that religious affinity.”
Assisted dying in Manitoba
In January 2018:
- 37 people reached out to the province’s Medical Assistance in Dying (MAID) team.
- Of those, 11 people died with the team’s help.
- Two of those people had to be transferred out of faith-based facilities in order to access MAID.
- Six people died sometime after reaching out to the team but without the team’s help.• Seven people were declined assistance by the MAID team for various reasons.
- There are currently 44 active cases.
In 2017:
- 314 people reached out the province’s Medical Assistance in Dying (MAID) team.
- Of those, 63 people died with the team’s help.
- 10 of those people had to be transferred out of faith-based facilities in order to access MAID.
- 87 people died sometime after reaching out to the team but without the team’s help.
- 52 people were declined assistance by the MAID team for various reasons.
Source: Winnipeg Regional Health Authority
That was made clear last June when the Catholic Health Corp. of Manitoba (CHCM) reshuffled the St. Boniface Hospital board in order to overturn a vote that would have allowed assisted dying on premises under limited circumstances.
Internal April 2017 memos from Dr. Marcus Blouw, the hospital’s medical staff president and board member at the time, made it clear there was staff support for such an amendment. Blouw had encouraged staff to reach out to him with their thoughts.
Of 65 responses with firm positions on the matter, the vast majority felt MAID needed to be available “to all Canadians, in any institution that receives public funding, regardless of that institution’s historical or religious affiliations.”
At the time, Blouw also registered concern about how many staff expressed worries to him about “the potential to suffer professional or personal repercussions for voicing strong opinions on this polarizing topic.”
He wrote to staff: “For myself, and for the majority of you who have chosen to speak to me about this over the past year, there is no debate: any practice that favours the sentiments of the institution over and above the needs of the patient would not be consistent with the stated mission, vision and goals of the hospital, nor does it foster good patient-physician relationships.”
When the board met near the end of May to consider a policy on MAID, it amended it to allow assisted dying on the premises in cases where a transfer would have been risky or ill advised. The amended policy narrowly passed, prompting the CHCM to add 10 new members to the board and “respectfully” ask for a re-vote since assisted dying, even in limited forms would be, “contrary to the ethical commitments of the health-care and social service organizations the CHCM controls.”
In his subsequent resignation letter, the then-St. Boniface board chairman Murray Kilfoyle said transfers were of serious concern: “I will be unable to support a policy I believe allows for the undeniable reality of transfers of care that harm patients.”
While the hospital’s then-chief executive officer (now chief medical officer of the WRHA) Dr. Bruce Roe said at the time that a plan for a new assisted-dying policy would be “shared in the coming weeks,” internal emails indicate patients continued to feel left in the lurch, their providers uncertain and hesitant — and not just at St. Boniface.
In a memo dated Sept. 29, Dr. Mike Harlos, head of the WRHA’s palliative-care program, wrote about stories from the provincial assisted-dying team about patients that “have felt abandoned and left to their own devices with regards to contacting the MAID team. This has left some feeling stigmatized because of their interest.”
Harlos went on to clarify that staff didn’t need to clear conversations or referrals for MAID with senior management; they could just provide the information. Still, he noted that it’s essential to have good communication.
“It’s important in each situation to be very clear who will be contacting — i.e. patient, family, or our staff — to avoid misguided assumptions that the other person is doing so.”
Faith-based, but respecting residents’ right to decide
Three faith-based personal cares homes in Winnipeg have opted to allow medical assistance in dying on site, citing the dignity and autonomy of their residents.
Three faith-based personal cares homes in Winnipeg have opted to allow medical assistance in dying on site, citing the dignity and autonomy of their residents.
The Saul and Claribel Simkin Centre, Luther Home, and Fred Douglas Lodge all allow residents to pursue and, if they’re eligible, receive medial assistance in dying (MAID) without having to leave their rooms.
“It all came down to this is their home and we provide resident-centred care,” said Keith Bytheway, chief executive officer at Luther Home. The Christ Lutheran Church founded the home in 1969 and while the Lutheran faith is still practised, that specific church is no longer in existence.
Luther Home spent six months or so consulting with its spiritual care committee and hearing from the provincial MAID team, as well as speaking with family members who had been through the process before reaching its decision.
“Although the faith may not support medical assistance in dying, the organization supports the residents and their choices,” Bytheway said. “This being a home, if people choose this path they’re choosing to do it in their own home and that seemed to be the deciding factor.”
Fred Douglas Lodge reached a similar conclusion over the course of several discussions, said CEO Roslyn Garofalo. The lodge is an affiliate of the United Church, whose philosophy centres on inclusivity.
“It wasn’t overly contentious,” she said. “We want to uphold people’s dignity as much as possible at the end of life.”
Although the Simkin Centre is not affiliated with a specific synagogue, CEO Irwin Corobow said it upholds Jewish values (the board is made up of members of Winnipeg’s Jewish community) such as honour, respect and compassion.
“We did not feel that in that case we would be honouring and respecting (residents) if we required them to move in order to access MAID.”
He stressed the Simkin Centre remains committed to conscientious objectors and will be working with the MAID team to facilitate any requests, but ultimately the question of whether to allow it came down to the notion of home.
“We wouldn’t ask them to leave their home,” Corobow said, and “this is the residents’ home.”
In making their choices, the three personal-care homes join a small cohort of faith-based facilities across the country that allow the full MAID process on site (only Quebec forces publicly funded, faith-based facilities to allow it).
“These organizations should be held up as models of putting the wishes, the rights and the choices of their residents first and foremost,” said Cory Ruf, a national spokesman with Dying with Dignity Canada.
The types of conversations that led the three Winnipeg personal care homes to make their choices could serve as a good model for dealing with issues of access in faith-based facilities and transfers moving forward, Ruf said.
Transfers have become a particularly charged issue this year, after it came to light a British Columbia doctor had provided medical assistance in dying to a patient in a faith-based personal care home despite clear directives from the facility not to do so.
Vancouver’s Louis Brier Home is, like Simkin Centre, a Jewish facility, one that operates in keeping with orthodox traditions and values that clearly stipulate no support for assisted dying.
“It was decided that while we respect residents’ wishes and recognize and value individuals’ decision making,” wrote Louis Brier’s CEO Dr. David Keselman in a memo to staff, “we would only agree to facilitate the MAID process on site to the point of assessment. Should the resident decide that they wish to pursue the process further, as an organization we would collaborate to facilitate the provision of the MAID process to be completed somewhere else.”
That’s not OK, said Dr. Ellen Wiebe, the physician who helped Louis Brier resident Barry Hyman die in his room. She would have helped two previous residents of the facility die in their rooms as well, she said, but at the last minute they decided they did want to be transferred out and the choice, she stresses, should be theirs.
“Remember, these are very vulnerable people, they are people who are very sick and they’re in a facility for a reason,” Wiebe said. “So, it’s really important that the facilities not take away other people’s rights and that’s what’s been happening.”
The Free Press obtained this memo along with other internal emails through a freedom of information request. St. Boniface Hospital initially tried to block the request, in part, on the basis it felt it had been “very open in sharing its position on medical assistance in dying with the media.” It reconsidered at the encouragement of the Manitoba Ombudsman.
Still, when it comes to sharing information about assisted dying, St. Boniface has its limits.
Hélène Vrignon, the hospital’s communication director, refused a request from a patient’s family late last August to put up a poster inviting patients to see a presentation about assisted dying offered by the MAID team.
In an email to the Free Press, Vrignon explained that, “While St. Boniface Hospital does not support the promotion of MAID via pamphlets, posters or presentations, we respond quickly and compassionately to requests made by patients and families when they seek information about MAID by directing them to the MAID team.”
But restricting pamphlets and posters is cause for concern, says Ruf.
“An information session does not mean that MAID is being promoted or advertised,” he says. “It’s alarming that a publicly funded institution would not even allow literature that would speak to the existence of an information session.”
Patients in St. Boniface won’t see pamphlets or posters, but that doesn’t mean conversations aren’t happening.
While Woods lay dying, his wife had many chats with the palliative-care staff working to make his death as peaceful as possible. They weren’t shy, she says, about sharing with her that they thought Woods should be allowed his assisted death and that others should be, too.
Karin Woods remembers thinking: these are the frontline workers. These are the people who know.
● ● ●
Leier is of the mind that where there are other options — other hospitals, other personal-care homes — requiring a patient to transfer out of a faith-based facility is OK.
You can’t impede a patient’s right to be processed for an assessment or a transfer, he says, but “it’s very difficult to say you need to be forced to do this, especially in a city like Winnipeg where there are many, many hospitals.”
That argument isn’t one Dr. Ellen Wiebe can abide.
She made headlines last month for helping a patient die in a Jewish personal-care home in British Columbia that explicitly does not allow it. She is unrepentant.
“They’re saying if you want MAID, go somewhere else… but that’s not how we deal with human rights,” Wiebe says. “If you’re a publicly funded facility and this is a legal medical procedure, then you have to be able to offer it or allow it.”

What Woods wishes is that her husband could have been allowed to plan ahead. It enrages her to think that he knew he wanted an assisted death and was in the process of obtaining it, but because he would have lost capacity during a transfer to a non faith-based facility, he wasn’t allowed to have it.
“It’s a mistake,” she says. “There should be a situation where you give your permission no matter what.”
They have to go back to the courts, Woods says, they have to address the uncertainties that have continued to permeate the assisted-dying debate even now, nearly two years after implementation of the federal law.
And they likely will, although Carissima Matthen, who teaches constitutional law at the University of Ottawa, says a case on faith-based transfers would take “a lot of time” to reach the Supreme Court.
It’s not necessarily a charter violation for faith-based facilities to exercise their medical judgment and say a patient such as George Woods is too ill for transfer, she says.
“But when its combined with the fact that the person, by virtue of their policy, is being forced to stay in a place where they are being denied something that the Supreme Court says they have a right to because of religious issues that shouldn’t be determining their health care,” Matthen says, “potentially, I think you do have a charter issue.”
● ● ●
There is a line in George Woods’ obituary that says he was fortunate not to need medical assistance in dying. It follows descriptions of skiing trips to Banff (he was a runner, a skier, energetic to a fault) and precedes plans for his son to scatter his ashes on one of his favourite slopes in Rossland, B.C.
His wife wrote it, although it’s not exactly what she wanted to say.
She is grateful, yes, that her husband died peacefully. But she wishes that he had died on his own terms.

The couple, married since 1963, had long followed the right-to-die debate in Canada. They’d watched as Sue Rodriguez, a Victoria, B.C., woman who suffered with amyotropic lateral sclerosis (ALS), pleaded her case before the Supreme Court, losing narrowly 5-4 in 1993, the same year a Gallup poll found that more than three-quarters of Canadians actually approved of assisted dying.
They kept paying attention decades later as Winnipegger Susan Griffiths wrote her own obituary before travelling to Switzerland to receive medical assistance in death in April 2013. In it, Griffiths laid out why “the CHOICE of death with dignity at a time determined by oneself and with qualified assistance should be available to everyone in Canada.”
Woods wishes her husband hadn’t been denied that choice. What she wishes had been published in his obituary is a description of the hospital room where he died. She wants people to see what he saw out his window: the Canadian Museum for Human Rights.
“How ironic,” she says.
jane.gerster@freepress.mb.ca
Twitter: @Jane_Gerster