Policy shift lands non-COVID patients in hospital units with active outbreaks
Advertisement
Read this article for free:
or
Already have an account? Log in here »
To continue reading, please subscribe:
Monthly Digital Subscription
$0 for the first 4 weeks*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*No charge for 4 weeks then price increases to the regular rate of $19.00 plus GST every four weeks. Offer available to new and qualified returning subscribers only. Cancel any time.
Monthly Digital Subscription
$4.75/week*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*Billed as $19 plus GST every four weeks. Cancel any time.
To continue reading, please subscribe:
Add Free Press access to your Brandon Sun subscription for only an additional
$1 for the first 4 weeks*
*Your next subscription payment will increase by $1.00 and you will be charged $16.99 plus GST for four weeks. After four weeks, your payment will increase to $23.99 plus GST every four weeks.
Read unlimited articles for free today:
or
Already have an account? Log in here »
Hey there, time traveller!
This article was published 29/04/2022 (1320 days ago), so information in it may no longer be current.
NON-COVID patients are being admitted to hospital units that have active outbreaks of the virus under a policy change that has received little public attention.
To free up acute-care capacity and reduce the number of emergency room patients waiting for a hospital bed, administrators changed outbreak admission guidelines in January, two months before the province lifted all COVID-19 public restrictions.
On Thursday, a Shared Health spokesperson stated hospitals do not track the number of patients who’ve been transferred into outbreak units. Four units had outbreaks at Health Sciences Centre as of Thursday afternoon.
The Jan. 13 guidance issued to health staff said it’s not always possible to avoid admitting patients who don’t have COVID-19 into areas with outbreaks, particularly if those patients need care in a specialized unit.
The policy recommends health professionals avoid placing unvaccinated patients, patients older than 60, or patients who are immunocompromised in outbreak units because of their increased risk of serious COVID-19 infection. It’s also not ideal, the guidance stated, to place new patients in units that have uncontained or newly declared outbreaks.
But the stretched-thin health-care system is not operating at an ideal level, and vulnerable people will suffer, says the family of a 90-year-old woman who is awaiting final test results after she was admitted to a Health Sciences Centre outbreak unit late last week. She has high-risk health conditions and shouldn’t have been placed with COVID-19 patients, her family says. On Thursday, the woman received a negative test result, but that hasn’t removed the family’s concerns. She will be tested again.
“It’s the weak who will perish; they (the government) don’t care,” said a family member who spoke on the condition of anonymity to protect the patient’s privacy. “If they cared, they wouldn’t be in this situation, putting a 90-year-old woman in a ward like that.”
The family found out the unit into which their relative had been transferred had been dealing with a COVID-19 outbreak since early April.
Shared Health stated patients with active COVID-19 infections are kept separate from patients who’ve never been infected with the virus, but may be kept distanced in the same general unit. The organization did not address the January memo, instead referring to a more detailed protocol, updated March 29, that links to the Jan. 13 guidance.
The January memo from Shared Health showed a change in practice from earlier pandemic protocols that aimed to keep non-COVID patients away from active outbreaks.
“It should be expected ward and/or facility outbreaks are going to increase in frequency and are not preventable. The approach being outlined herein is to allow for a balance of staff/patient/resident safety while maximizing our acute care capacity and permitting ongoing delivery of complex co-ordinated care for patients. Acute care sites can no longer suspend admissions to a unit/site that is in outbreak,” the Jan. 13 Shared Health memo states.
The day before the memo was issued, Premier Heather Stefanson spoke publicly about the need for Manitobans to “look after themselves.”
“We must all learn to live with this virus; there must be a balance,” Stefanson said at the time.
“What it really means, for the vulnerable, is we have to learn to die with it,” the patient’s family member said.
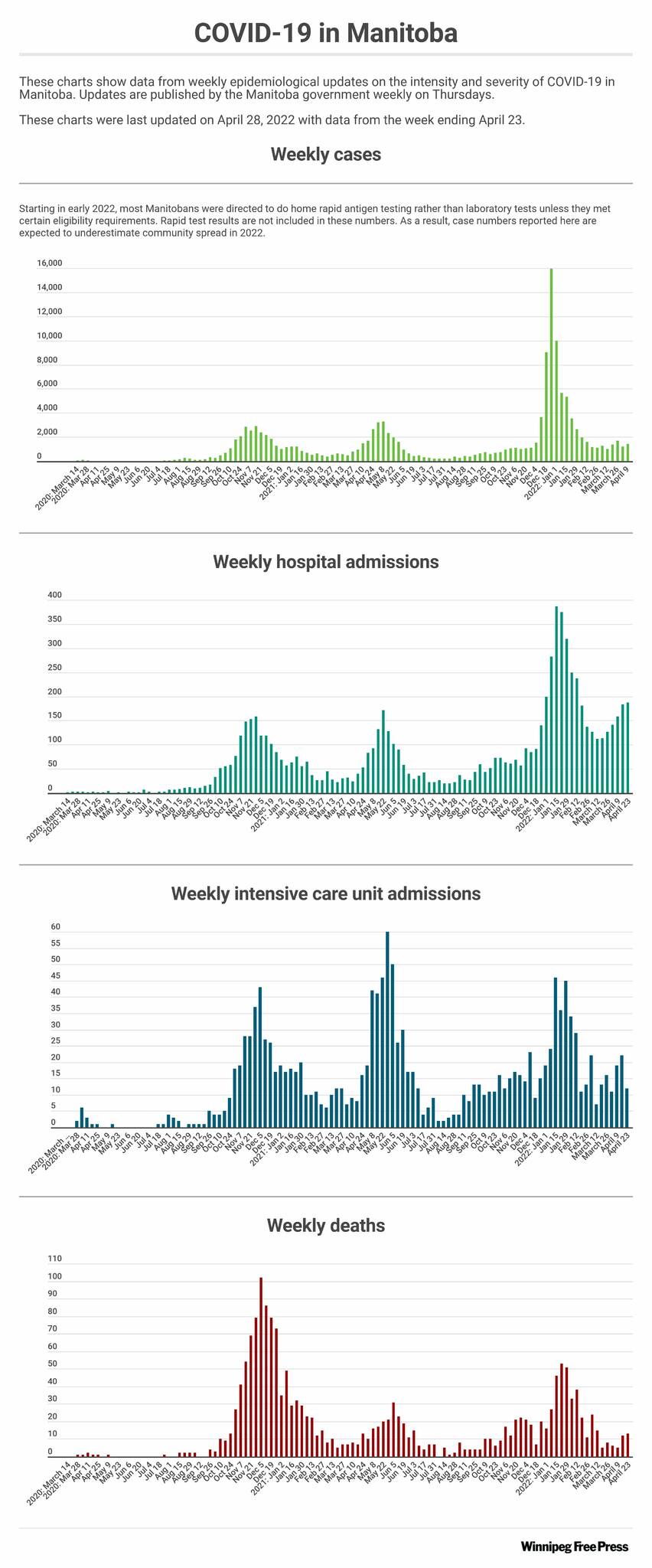
After three consecutive weeks of increasing COVID-19 hospital admissions, the number of COVID-19 patients has dropped slightly.
Two-hundred Manitobans were hospitalized with COVID-19 and there were 13 deaths from the virus last week, according to the latest figures released by the provincial government.
The province’s epidemiological report for April 17 to April 23 showed 12 of the 200 hospitalizations were intensive-care admissions. That’s compared to 206 hospitalizations, 22 ICU admissions, and 12 deaths during the previous week, from April 10 to 16.
Although most Manitobans don’t have access to PCR testing, test positivity rates are increasing for those getting lab-confirmed PCR results. An average of 955 Manitobans per day receive PCR tests, and the test positivity rate is at 23.4 per cent, up from 19 per cent a week earlier.
As of last week, Shared Health said there are two designated COVID-19 hospital units, one in Winnipeg and one in Brandon. All patients are tested upon admission. Those who test positive are grouped together or with recovered COVID-19 patients; those with suspected cases of the virus are isolated until results are confirmed.

katie.may@winnipegfreepress.com

Katie May is a general-assignment reporter for the Free Press.
Our newsroom depends on a growing audience of readers to power our journalism. If you are not a paid reader, please consider becoming a subscriber.
Our newsroom depends on its audience of readers to power our journalism. Thank you for your support.