Testing questioned as Manitoba COVID-19 cases spike
Read this article for free:
or
Already have an account? Log in here »
To continue reading, please subscribe:
Monthly Digital Subscription
$0 for the first 4 weeks*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*No charge for 4 weeks then price increases to the regular rate of $19.00 plus GST every four weeks. Offer available to new and qualified returning subscribers only. Cancel any time.
Monthly Digital Subscription
$4.75/week*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*Billed as $19 plus GST every four weeks. Cancel any time.
To continue reading, please subscribe:
Add Free Press access to your Brandon Sun subscription for only an additional
$1 for the first 4 weeks*
*Your next subscription payment will increase by $1.00 and you will be charged $16.99 plus GST for four weeks. After four weeks, your payment will increase to $23.99 plus GST every four weeks.
Read unlimited articles for free today:
or
Already have an account? Log in here »
Hey there, time traveller!
This article was published 25/03/2020 (2091 days ago), so information in it may no longer be current.
Kerry Smith was at the same Vancouver conference hall as multiple people who later tested positive for COVID-19 and a B.C. dentist who died this week.
That thought has been weighing heavily on her mind since she became ill after returning home to Manitoba and began experiencing a significant shortness of breath. However, repeated efforts to get tested for the novel coronavirus resulted only in frustration — leaving her worried many more Manitobans may unknowingly be infected.

“To say that we have 35 people infected? That’s ridiculous, we have way more than that,” Smith said Wednesday.
Smith, who works for the Manitoba Metis Federation, attended an event in the same facility as the Pacific Dental Conference March 5-7. By March 16, her symptoms had worsened. She called Health Links provincial telephone info service several times, but couldn’t get through. She contacted a private nurse, who told her she should be tested for COVID-19.
At the Winnipeg testing site, Smith said she was turned away because she had not travelled internationally. Fearing she might have COVID-19, Smith took extra precautions, pulled her children out of school and her husband stayed home from work to self-isolate.
“I could very easily have taken the attitude: if the province isn’t worried then why am I? And I assure you there are people who did,” she said.
By March 20, her symptoms had persisted, and she was tested at the Selkirk screening site. Smith is still waiting for the results.
wfpsummary:Dr. Joel Kettner, who oversaw Manitoba’s response to large outbreaks as the province’s public health chief from 1999 to 2012, said what public health officials want from testing numbers and what the public want from numbers are two different things.:wfpsummary
Dr. Joel Kettner, who oversaw Manitoba’s response to large outbreaks as the province’s public health chief from 1999 to 2012, said what public health officials want from testing numbers and what the public want from numbers are two different things.
Kettner said the reasons someone would be tested would have to fall into three categories.
First, does a positive result mean that a patient would experience different treatment from health professionals? In all COVID-19 cases, the answer is ‘no,’ because there is no current treatment for the novel coronavirus.
Second, he said there’s an argument for testing to decide if a person should be isolated or not. As everyone is advised to stay home, this is less important right now. But this is a reason to test health-care professionals who need to get back to work but may be exhibiting symptoms.
Surveillance is the third reason to test people, which results in more information about the epidemic.
“There’s lots of things we want to know about this epidemic, of which community spread is one of them. But some people might make the argument that it is not the most important thing,” Kettner said, adding what is likely more important is understanding the characteristics of those who are being hospitalized, those who need intensive care, and those who die.
“I don’t care that much about asymptomatic people and people with mild (symptoms), other than the potential of them spreading it to others. I’m not worried about those people themselves. I am worried about the people who are sick enough to go to hospital or the ICU,” Kettner said.
Outside of hospitals, Kettner said if the province was adequately testing those who had travelled and those who had contact with those who travelled, it would give public health authorities a sufficient amount of information about spread.
“If you want to know better what is the amount of community spread — in other words, how many people are sick that we’re not testing, because they don’t fit these categories — the place to test those people is in the hospital (when they present) with acute respiratory illness,” Kettner said.
“They’re the ones I want to know where they’re getting it.”
A recent survey conducted by polling firm Leger underlined how difficult widespread testing would be. Of 1,508 respondents to the survey, 18 per cent of people answered they exhibited at least one of the symptoms related to COVID-19, but likely unconnected.
— Sarah Lawrynuik
“I don’t know what it costs to test people. But I’m more worried about what it costs to not test people.”
On March 16, the 15,000 people who had attended the dental conference — in the same location where Smith had been — were told to self-isolate by B.C.’s public health officer, who confirmed several cases of COVID-19 had been traced to the event. Vancouver dentist Denis Vincent, who was in his 60s, died on the weekend.
Dr. Alan Katz, director of the Manitoba Centre for Health Policy, said while there are reasons testing is limited, more screening is vital to track and keep a lid on the pandemic.
“What is the true community-based prevalence of infection?” Katz said. “The only way to do that is through a mass, broad-testing approach… That’s key information to make much more informed policy decisions.”
Manitoba has limited testing to the most at-risk groups; it has also been hamstrung by a backlog at the Cadham Provincial Laboratory.
The messaging of who should be tested isn’t consistent and getting to everyone, Katz said. He pointed to examples of people being referred for COVID-19 testing by one public health worker at Health Links only to be turned away at the testing site by another public health worker.

“It depends on where you go,” he said. “You might get a test. You might be turned away.”
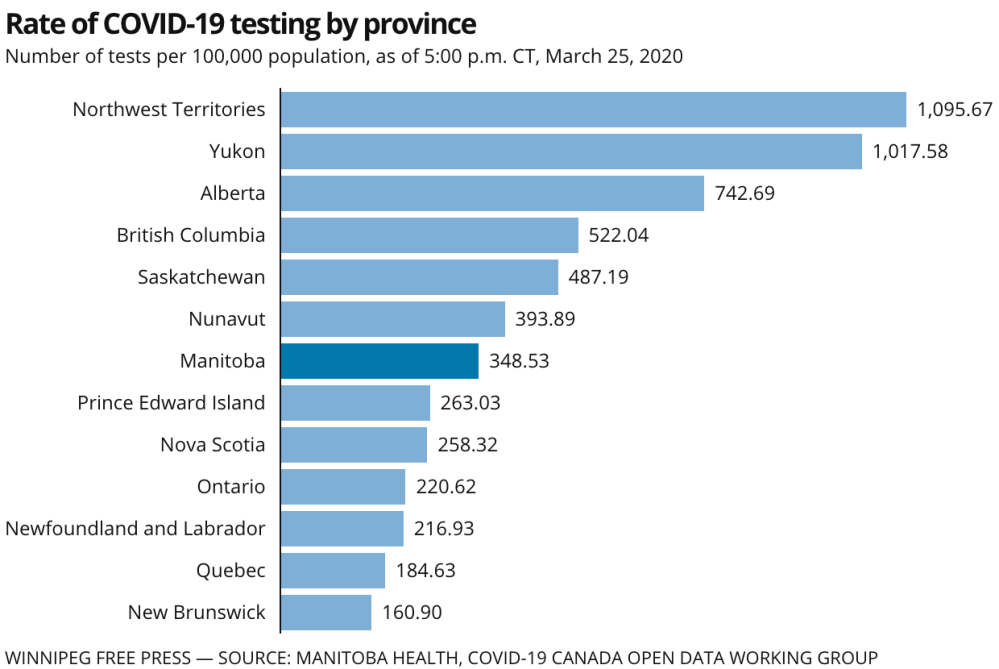
In Saskatchewan, more than 5,700 people were tested as of Tuesday, with at least 72 presumptive and confirmed cases of COVID-19. However, it’s difficult to compare why the province next door — with a similar population and geographic size — has twice as many cases as Manitoba, partly because the testing has been inconsistent, Katz said.
“When we look at what’s happening across the country, we know very little,” said Katz. “If in Manitoba, we’re not consistently applying standards for testing, you can imagine across Canada.
“This results in the actual number of positive tests not being comparable across the country. We don’t know where we are in the curve compared to other provinces and places.”

When testing began in February, all returning international travellers to Manitoba who developed cold- or flu-like symptoms within 14 days were told to self-isolate and contact Health Links to see if they should be tested. Now, Manitoba is prioritizing the most at-risk groups for testing.
Only those Manitobans with respiratory symptoms who have travelled out of province in the past 14 days or who have had direct contact with confirmed or suspected COVID-19 cases at large events (conferences, cruises, flights) need to be tested at this time, the province said.
Health Minister Cameron Friesen said Wednesday First Nations — hit hard by the 2009 H1N1 epidemic — are also prioritized for testing.
Katz said Manitoba learned from the H1N1 outbreak, when the rate of hospitalization for First Nations was seven times higher than the rest of the province.
“We learned lessons, not in terms of testing, but in terms of how it can affect needs in different parts of the province.”
carol.sanders@freepress.mb.ca
sarah.lawrynuik@freepress.mb.ca

Our newsroom depends on a growing audience of readers to power our journalism. If you are not a paid reader, please consider becoming a subscriber.
Our newsroom depends on its audience of readers to power our journalism. Thank you for your support.
History
Updated on Thursday, March 26, 2020 9:26 PM CDT: Updates lede of story to remove reference to dentist having virus.